VLDL (Very Low-Density Lipoprotein) Test: Meaning, Normal Range, Causes, Symptoms, and Complete Guide
What is VLDL (Very Low-Density Lipoprotein)?
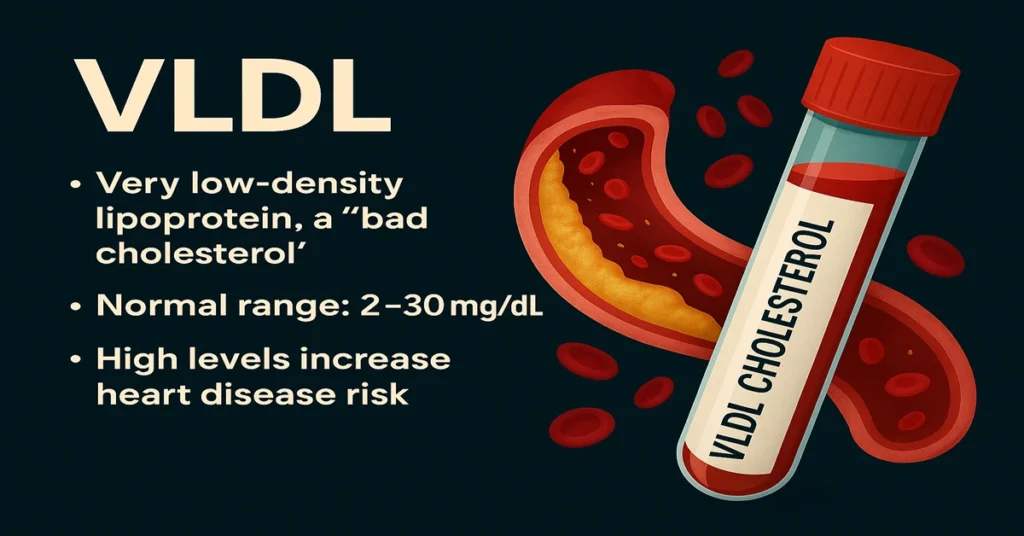
VLDL stands for Very Low-Density Lipoprotein. It is one of the particles that transport fats through the bloodstream and is commonly grouped under “bad cholesterol.” While LDL is more widely discussed, VLDL also plays an important role in cardiovascular risk, especially when triglyceride levels are elevated.
VLDL mainly carries triglycerides, which are fats formed from excess calories, sugars, carbohydrates, and alcohol. When triglycerides rise, VLDL levels usually rise along with them. For this reason, VLDL offers doctors a useful window into metabolic health and long-term heart risk.
In normal amounts, VLDL is part of everyday fat transport. When levels remain high for long periods, however, these particles contribute to fat deposition within blood vessel walls, gradually narrowing arteries and affecting circulation.
Where is VLDL Produced in the Body?
VLDL is produced almost entirely in the liver. The liver assembles triglycerides, cholesterol, and specific proteins into VLDL particles and releases them into the bloodstream.
Once in circulation, VLDL participates in a natural conversion process. As it delivers triglycerides to muscles and fat tissue, the particle becomes smaller and denser. It first changes into intermediate-density lipoprotein (IDL) and is later converted into LDL.
This stepwise transformation explains why elevated VLDL levels are often seen together with high LDL and why both are considered relevant when assessing cardiovascular risk.
Functions and Importance of VLDL
Although VLDL is often labeled harmful, it serves several necessary metabolic functions when present in balanced amounts.
Its primary role is the transport of triglycerides from the liver to tissues that require energy. Between meals or during increased physical demand, these triglycerides are used as fuel. VLDL also supports the body’s ability to store excess energy safely for later use.
From a clinical perspective, VLDL matters because it sits at the crossroads of triglyceride metabolism and cholesterol transport. When production exceeds the body’s needs, this balance shifts, and vascular damage can slowly develop.
Causes of Low VLDL Levels
Low VLDL levels are uncommon and usually not a cause for concern. In most cases, they reflect efficient fat metabolism rather than disease.
Situations where VLDL may appear low include conditions that reduce liver fat production, increase metabolic rate, or limit nutrient intake. Doctors generally interpret low VLDL values in the context of overall health, other lipid results, and clinical findings rather than as an isolated abnormality.
Symptoms of Low VLDL
Low VLDL itself does not usually cause symptoms. When extremely low values are seen, they are typically related to underlying metabolic or genetic conditions rather than the lipoprotein level alone. In routine practice, low VLDL is often viewed as a neutral or favorable finding.
Causes of High VLDL Levels
High VLDL levels are much more common and usually reflect elevated triglycerides. This pattern is frequently seen in metabolic conditions and lifestyle-related disorders.
From a laboratory viewpoint, high VLDL suggests increased liver production of triglyceride-rich particles or reduced clearance from circulation. Conditions affecting glucose regulation, thyroid function, liver health, or kidney function may contribute. Certain medications and inherited lipid disorders can also influence VLDL levels.
Because VLDL closely mirrors triglyceride behavior, factors that raise triglycerides tend to raise VLDL as well.
Symptoms of High VLDL
VLDL itself does not produce symptoms. Any symptoms that appear are usually related to long-term effects of fat buildup in blood vessels or complications of very high triglycerides.
These effects develop gradually and may involve the heart, brain, liver, or peripheral circulation. This delayed presentation is why VLDL is primarily valued as a preventive marker rather than a diagnostic tool for immediate symptoms.
Reference Range (Normal Values)
VLDL is usually calculated from fasting triglyceride levels using the standard formula:
VLDL = Triglycerides ÷ 5
(This calculation is reliable when triglycerides are below 400 mg/dL.)
Common reference interpretation:
- 2–30 mg/dL: Typical range
- Above 30 mg/dL: Elevated and associated with increased cardiovascular risk
Clinicians usually interpret VLDL alongside triglycerides, LDL, and HDL rather than on its own.
Sample Type
Sample Type: Serum
Tube Used: Red top (plain tube)
VLDL assessment is part of a standard fasting lipid profile.
Test Preparation
Accurate measurement generally requires short-term fasting. Alcohol intake, recent dietary changes, and certain medications can temporarily influence triglycerides and VLDL levels. Patients are usually advised to maintain their usual routine before testing rather than making abrupt changes.
When to Consult a Doctor
Medical review is advised when VLDL remains elevated on repeat testing or appears alongside other abnormal lipid values. Individuals with diabetes, high blood pressure, obesity, fatty liver, or a family history of heart disease benefit from regular lipid monitoring.
Doctors use VLDL results as part of an overall metabolic and cardiovascular assessment, guiding further evaluation when needed.
Important Word Explanations
- Lipoprotein: A particle made of fats and proteins that transports lipids through the blood.
- Triglycerides: A form of stored fat derived from excess calories and used for energy.
- Atherosclerosis: Gradual narrowing of arteries due to fat and cholesterol buildup.
- IDL: An intermediate particle formed during the conversion of VLDL into LDL.
- Metabolic Syndrome: A cluster of conditions that increases the risk of heart disease and diabetes.
~END~