RBC Count Normal but Hematocrit Low – Lab Interpretation Explained
A report combination that confuses many patients (and even students)
In OPD and diagnostic lab practice, one question comes up very often:
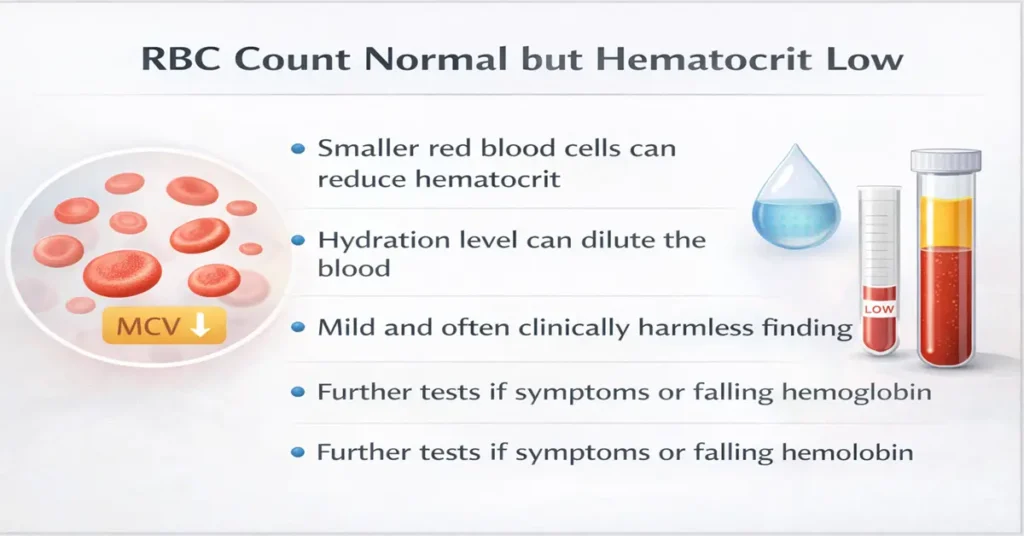
“My RBC count is normal, but hematocrit is low. What does that mean?”
At first glance, it feels contradictory. If the number of red blood cells (RBCs) is normal, then why is hematocrit (HCT or PCV) showing low?
From real hospital and lab experience, I can say this clearly: this combination is usually explainable, often harmless, and very commonly seen in routine reports.
This article focuses only on this specific lab pattern. It does not repeat basic test meanings, normal ranges, or disease lists. The goal is to help you understand how this happens and how doctors interpret it in real practice.
Understanding the confusion in simple words
RBC count tells us how many red blood cells are present in the blood sample.
Hematocrit tells us how much space those red blood cells occupy in the blood.
So even if the number of cells is normal, the total volume occupied by those cells can be lower. That is where this mismatch comes from.
In simple terms:
- RBC = number of cells
- Hematocrit = size + volume of those cells
When doctors see this pattern, they don’t see it as a contradiction. They see it as a volume-related issue, not a number problem.
Why this happens in real-world lab practice
From years of reading CBC reports and discussing them with doctors, this situation usually happens due to practical and physiological reasons, not serious illness.
Let’s go through the most common ones.
1. Smaller-sized red blood cells (very common finding)
This is the most frequent reason for normal RBC count with low hematocrit.
If red blood cells are:
- Slightly smaller in size
- But present in normal numbers
Then:
- RBC count stays normal
- Hematocrit becomes low because total volume is reduced
In lab terms, this often goes along with a lower MCV value.
From OPD experience, this pattern is seen in many patients who:
- Feel completely fine
- Have no symptoms
- Are picked up only during routine testing
Clinically, doctors usually correlate this with other indices and often just observe.
2. Mild dilution of blood (hydration-related)
Hematocrit is very sensitive to hydration status.
When a patient is:
- Well hydrated
- Or has taken excess fluids before the test
The plasma portion of blood increases. This causes:
- RBC count to remain stable
- Hematocrit to appear slightly low
In lab discussions, this is often described as:
“Dilutional effect.”
This is common in:
- Hospitalized patients
- People tested after IV fluids
- Individuals who drank a lot of water before testing
In such cases, doctors usually don’t worry at all.
3. Recent illness or recovery phase
After:
- Fever
- Viral infection
- Minor illness
The body’s fluid balance and red cell dynamics change temporarily.
During recovery:
- RBC number may normalize quickly
- Hematocrit may lag behind slightly
From lab experience, this temporary mismatch corrects itself over time.
That is why doctors often ask:
“Recent illness ya fever hua tha?”
4. Borderline values and reference cutoffs
Many times, hematocrit is only:
- Slightly below the reference range
- Just a fraction lower
In such cases:
- RBC count sits comfortably in normal range
- Hematocrit crosses the cutoff by a small margin
Clinically, this is often reported as:
“Borderline low, not significant.”
Doctors do not treat numbers in isolation. They treat patterns.
5. Lab and analyzer-related variation
From inside-the-lab experience, hematocrit can vary due to:
- Analyzer calculation method
- Sample mixing quality
- Time delay between collection and testing
Modern analyzers often calculate hematocrit, not measure it directly.
So small variations can occur even when RBC count is stable.
This is considered acceptable and normal in laboratory medicine.
How doctors usually interpret this combination
In OPD practice, doctors rarely react to hematocrit alone.
They usually check:
- Hemoglobin trend
- RBC indices
- Patient symptoms
- Clinical background
If:
- RBC count is normal
- Hemoglobin is stable
- Patient has no symptoms
Doctors often conclude:
“No active concern. Observe.”
This combination is usually interpreted as a mild volume or cell-size issue, not anemia or disease.
When this finding is usually harmless
From long lab experience, this pattern is usually harmless when:
- The patient feels well
- Hemoglobin is stable
- RBC count is normal
- Platelets and WBC are normal
- Hematocrit is only mildly low
In such cases, no urgent action is taken.
When doctors pay closer attention
Doctors become more alert when this pattern is seen along with:
- Falling hemoglobin on repeat tests
- Symptoms like fatigue or breathlessness
- Significant drop in hematocrit over time
- Abnormal trends in other CBC parameters
Even then, decisions are based on overall trend, not a single report.
Should you repeat the test?
From routine lab protocol, repeat testing is advised when:
- The test was done during illness or hospitalization
- Hydration status was abnormal
- Doctor wants to confirm a trend
Repeat testing is usually not required immediately when:
- You feel fine
- Hemoglobin is normal
- Doctor is clinically satisfied
Unnecessary repeat tests often create more confusion.
A common mistake patients make
Many patients:
- Focus only on the “low” mark
- Compare reports line by line
- Panic after online searches
In lab practice, we often reassure patients by saying:
“RBC theek hai, Hb stable hai, sirf HCT thoda low hai – clinically koi problem nahi.”
Context always matters more than one value.
What this report does NOT automatically mean
This pattern does not automatically indicate:
- Serious anemia
- Internal bleeding
- Bone marrow disease
- Chronic illness
Those conditions usually show multiple abnormal parameters and symptoms, not isolated hematocrit changes.
Test Preparation
To avoid misleading hematocrit values in future tests:
- Maintain normal hydration (not excess, not too little)
- Avoid heavy exercise just before testing
- Give blood in a rested state
- Inform the lab about recent illness or IV fluids
Good preparation improves report consistency.
When to Consult a Doctor
Consult your doctor if:
- You have ongoing fatigue or breathlessness
- Hematocrit keeps falling on repeat tests
- Hemoglobin also starts decreasing
- You have a known blood disorder
Otherwise, mild low hematocrit with normal RBC is usually not alarming.
Important Word Explanations
RBC (Red Blood Cell): Cells that carry oxygen in blood.
Hematocrit (HCT / PCV): Percentage of blood volume occupied by red blood cells.
MCV: Average size of red blood cells.
Dilutional effect: Lower concentration due to increased fluid in blood.
CBC: Complete Blood Count test.
People Also Ask
Can hematocrit be low even if RBC count is normal?
Yes. This commonly happens when red blood cells are smaller or blood is diluted.
Is low hematocrit always anemia?
No. Doctors correlate it with hemoglobin and symptoms before calling it anemia.
Should I worry if only hematocrit is low?
Usually no, especially if RBC count and hemoglobin are stable.
Does hydration affect hematocrit more than RBC count?
Yes. Hematocrit is more sensitive to fluid changes.
~END~