Normal Range of Alcohol Test
Why Normal Range Matters
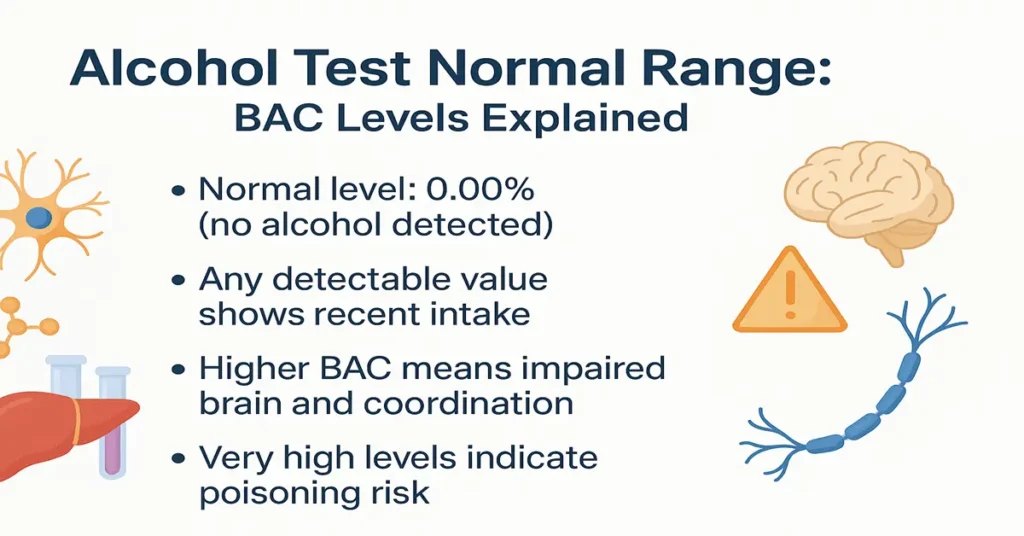
The alcohol test measures how much alcohol is present in the blood at a specific moment, most commonly reported as Blood Alcohol Concentration (BAC). Unlike many laboratory parameters, alcohol does not have a “healthy” or desirable level. In routine medical practice, the expected normal value is simply zero.
Understanding the normal range matters because even small amounts of alcohol can affect judgment, coordination, reaction time, and decision-making. Clinically, doctors use this information to decide whether symptoms such as confusion, drowsiness, poor balance, vomiting, or altered behavior are likely related to alcohol or whether another medical problem needs urgent attention.
Correct interpretation also plays a role in emergency care, workplace screening, legal evaluation, and monitoring patients with alcohol-related health issues. Knowing what is normal helps avoid confusion and supports safer clinical decisions.
General Reference Range
In medical laboratories, the normal reference range for an alcohol test is:
0 mg/dL or 0.00% BAC
This indicates that no alcohol is detected in the blood.
Any value above zero means alcohol has been consumed recently. Laboratories usually report results in milligrams per deciliter (mg/dL) or as a percentage (% BAC). For clinical understanding, alcohol levels are often grouped as follows:
- 0 mg/dL (0.00%) – No alcohol detected
- 1–50 mg/dL (0.01–0.05%) – Mild effects, reduced alertness
- 50–100 mg/dL (0.05–0.10%) – Impaired coordination and judgment
- 100–200 mg/dL (0.10–0.20%) – Clear intoxication
- Above 200 mg/dL (0.20%) – High risk of alcohol poisoning
In practice, these ranges help doctors estimate severity, but they do not define what is “safe.” Individual response varies widely.
Age-Wise Normal Range
There is no separate age-based normal range for alcohol testing. The expected normal value is zero at all ages. What changes with age is how the body handles alcohol.
In children and adolescents, any detectable alcohol level is considered abnormal and concerning. Even small amounts can cause significant symptoms because metabolism is immature and tolerance is low. Detection in this age group often prompts evaluation for accidental ingestion or exposure.
In adults, metabolism depends on liver health, body composition, and drinking habits. Older adults generally process alcohol more slowly due to reduced liver efficiency and lower muscle mass. As a result, the same intake may lead to higher blood levels, even though the normal reference value remains unchanged.
Gender-Wise Normal Range
The laboratory normal range is the same for males and females: 0 mg/dL. However, gender influences how alcohol behaves in the body.
On average, women tend to reach higher blood alcohol levels than men after consuming the same amount. This is related to differences in body water content, enzyme activity, and hormonal factors. Women often experience stronger effects at lower levels, even though the test interpretation uses the same reference range for both sexes.
Clinically, doctors keep this in mind when correlating test results with symptoms.
Pregnancy-Specific Normal Range
During pregnancy, the normal range remains 0 mg/dL, and any detectable alcohol is considered unsafe. There is no known safe level of alcohol exposure during pregnancy.
Alcohol crosses the placenta easily and can affect fetal brain development, even at low levels. For this reason, alcohol testing in pregnancy is interpreted with extra caution, and any positive result requires counseling and follow-up. Routine testing is not standard, but it may be done in specific medical situations.
Factors That Affect Test Values
Several factors influence alcohol levels and their interpretation. The most important are the amount consumed and the time since the last drink. Alcohol usually peaks within 30 to 90 minutes, depending on food intake.
Drinking on an empty stomach leads to faster absorption and higher peak levels. Body weight, muscle mass, and hydration status also matter. People with lower body weight or less muscle mass often show higher BAC for the same intake.
Liver health plays a major role. Fatty liver, hepatitis, or cirrhosis slow alcohol breakdown, causing levels to stay elevated longer. Certain medications can interfere with metabolism or intensify alcohol’s effects.
The test method also matters. Blood testing is the most accurate. Breath and urine tests are useful for screening but may vary based on timing and conditions.
Additional Information
Once drinking stops, alcohol levels usually fall at a steady rate, often around 15–20 mg/dL per hour in many adults. This rate varies and cannot be safely accelerated. Coffee, cold showers, or exercise may increase alertness but do not reduce blood alcohol levels.
Tolerance does not change the measured value. Someone who appears “fine” may still have a high BAC. In medical settings, numbers and symptoms together guide decisions, not appearance alone.
Alcohol tests are frequently ordered along with liver function tests, blood sugar, and electrolytes to build a clearer clinical picture.
Test Preparation
If testing is planned, patients are usually advised to avoid alcohol for at least 24 hours unless the goal is to detect recent intake. Always inform the healthcare provider about recent drinking, medications, and existing medical conditions.
No fasting is required specifically for an alcohol test. In emergencies, no preparation is needed and testing is done immediately.
When to See a Doctor
A doctor should be consulted if alcohol test results are unexpectedly high, repeatedly positive, or linked with symptoms such as confusion, dizziness, vomiting, or fainting. Immediate medical care is required for signs of alcohol poisoning, including slowed breathing, seizures, or unresponsiveness.
People with liver disease, pregnancy, or difficulty controlling alcohol use should seek medical advice even at lower levels. Early evaluation helps prevent serious complications.
Sample Type
Alcohol levels are most accurately measured using a blood sample drawn from a vein. Breath or urine samples may be used for screening or legal purposes, but blood testing is preferred for medical evaluation.
Important Word Explanations
Blood Alcohol Concentration (BAC): The amount of alcohol present in the blood at a given time.
mg/dL: Milligrams per deciliter, a unit used to measure blood concentration.
Alcohol Dehydrogenase: A liver enzyme that breaks down alcohol.
Alcohol Poisoning: A dangerous condition caused by extremely high alcohol levels.
Tolerance: Reduced visible effects of alcohol despite high blood levels due to repeated exposure.
People Also Ask
Is a positive alcohol test always serious?
Not always. Low levels may cause mild effects, but higher values can be dangerous and need medical attention.
Can alcohol levels be temporary?
Yes. Alcohol levels rise after drinking and usually fall as the liver processes alcohol over time.
Does a normal result rule out alcohol problems?
No. It only shows there was no recent alcohol intake, not long-term drinking habits.
When do doctors usually worry about alcohol levels?
When levels are high or symptoms like confusion, breathing problems, or loss of consciousness appear.
Is repeat testing common?
Yes. In hospitals, repeat tests are often done to monitor clearance and patient safety.
Do coffee or cold showers lower alcohol levels?
No. They may increase alertness but do not reduce alcohol in the blood.
~END~

Hi, i think that i saw you visited myy blog thus i came to “return the favor”.
I am trying to find things to enhance my site!I suppose its ok to use same of your ideas!!