Normal Range of ADH Test
The ADH test measures the level of antidiuretic hormone, also known as vasopressin, in the blood. ADH is a key hormone that controls how the body manages water by regulating how much water the kidneys retain and how much is passed out in urine. Because this hormone works in very small concentrations, even minor changes can disturb fluid balance and sodium levels.
In routine lab practice, ADH is not treated like a simple “normal or abnormal” test. Its value always needs to be interpreted alongside symptoms, hydration status, sodium levels, and urine findings. Understanding the normal range helps clinicians decide whether the hormone regulation system is working as expected or needs further evaluation.
Why Normal Range Matters
The normal range of the ADH test gives doctors a reference point to judge whether the hypothalamus, pituitary gland, and kidneys are communicating properly. When ADH values fall within the expected range, it usually suggests that water regulation is functioning in a balanced way.
When ADH is too low or too high, the body’s water handling becomes abnormal. Clinically, this may show up as excessive urination, persistent thirst, water retention, swelling, or abnormal sodium levels. Because these symptoms overlap with many other conditions, the normal range provides an objective anchor for interpretation.
In real-world practice, ADH results are especially helpful in patients with unexplained electrolyte imbalance, abnormal urine output, or neurological symptoms where fluid regulation is suspected to be part of the problem.
General Reference Range
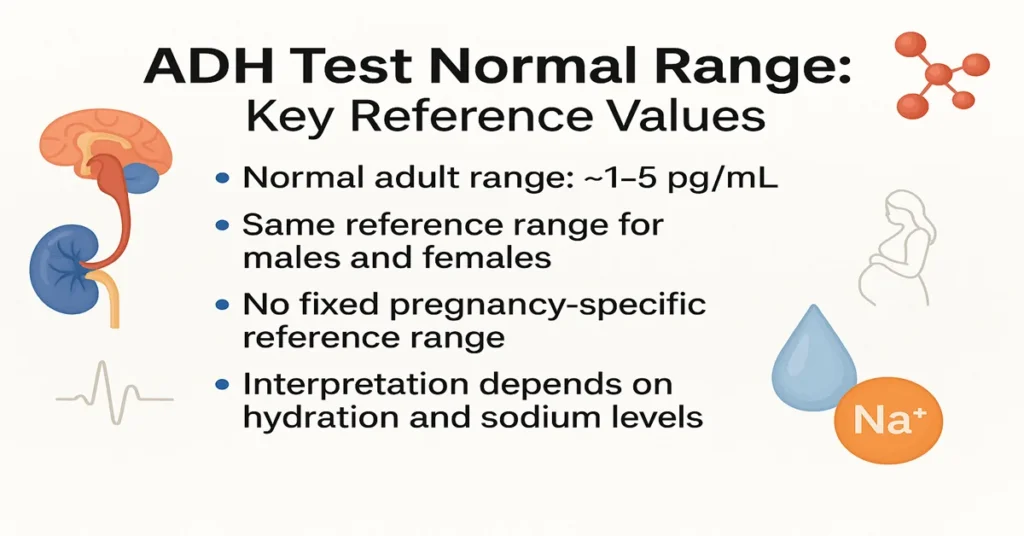
Under standard testing conditions, the commonly accepted adult reference range for ADH is approximately:
1 to 5 pg/mL (picograms per milliliter)
This range applies to blood samples collected under controlled conditions. However, ADH is highly sensitive to several factors, including hydration, posture, stress, and timing of sample collection.
Different laboratories may use slightly different methods, which can lead to minor variations in reference ranges. For this reason, clinicians always rely on the reference range printed on the individual lab report rather than a fixed universal number.
Values below the reference range may act as a signal of reduced ADH production or release, while values above the range may point toward excess secretion or inappropriate regulation. On their own, these values are not diagnostic and must be correlated with other findings.
Age-Wise Normal Range
There is no strictly defined age-specific ADH reference range used in routine clinical practice, but age-related changes influence how results are interpreted.
In children, ADH control mechanisms are still maturing. Pediatric results are interpreted cautiously and usually in the context of symptoms rather than numbers alone.
In adults, ADH levels are generally stable, and the standard reference range is applied.
In older adults, thirst sensation and kidney responsiveness may decline. ADH values may still fall within the normal range, but the body’s response to the hormone can be altered. Clinically, this is why elderly patients may develop dehydration or water retention even with borderline values.
Doctors usually focus more on sodium levels, urine concentration, and symptoms than on age-based cutoffs.
Gender-Wise Normal Range
There is no clinically significant difference in ADH reference ranges between males and females. Both sexes use the same normal values when tested under similar conditions.
Hormonal fluctuations in women, especially related to estrogen, can subtly influence water retention, but these changes are usually physiological and do not require separate reference ranges.
In practice, gender does not change how ADH results are interpreted. Clinical context remains far more important than sex-based differences.
Pregnancy-Specific Normal Range
Routine ADH testing during pregnancy is uncommon, and there is no clearly defined pregnancy-specific reference range.
Pregnancy naturally increases blood volume and alters fluid handling. These changes can influence ADH activity without indicating disease. Mild shifts in values may still represent normal physiology during pregnancy.
Because of this, ADH test results in pregnant individuals are interpreted very cautiously and always alongside symptoms, sodium levels, and other investigations. Testing is usually done only when there is a clear clinical reason.
Factors That Affect Test Values
ADH levels are easily influenced by several internal and external factors, which is why test preparation and context matter so much.
Hydration status plays a major role. Excessive water intake before testing can temporarily suppress ADH, while dehydration can raise it.
Body posture affects results. ADH levels may differ depending on whether the patient was lying down, sitting, or standing at the time of collection.
Stress, pain, anxiety, and acute illness can stimulate ADH release. This is commonly seen in hospitalized patients.
Medications such as antidepressants, antipsychotics, seizure medicines, chemotherapy drugs, and some pain medications can alter ADH secretion or its effect on the kidneys.
Underlying conditions involving the lungs, brain, kidneys, or endocrine system can also influence results. For this reason, ADH values are never interpreted in isolation.
Additional Information
In clinical practice, ADH testing is almost always paired with serum sodium, plasma osmolality, urine osmolality, and urine sodium. These combined results provide a clearer picture of water balance than any single test.
In some situations, dynamic testing under controlled conditions may be needed to clarify borderline or confusing results. Imaging of the brain or pituitary gland may also be advised if abnormalities are suspected.
It is important to understand that a value slightly outside the normal range does not automatically mean disease. Repeat testing and clinical correlation are often necessary.
Test Preparation
Proper preparation improves the accuracy of ADH testing. Patients are usually advised not to drink excessive amounts of water before the test, as overhydration can falsely lower ADH levels.
Some medications may need adjustment before testing, but this should only be done after consulting a doctor. Medications should never be stopped without medical advice.
In certain cases, fasting or controlled fluid intake may be required, especially when ADH testing is part of a broader diagnostic evaluation.
When to See a Doctor
Medical advice should be sought if symptoms such as excessive thirst, frequent urination, unexplained fatigue, confusion, swelling, or persistent headaches are present.
Urgent medical attention is needed if there are signs of severe electrolyte imbalance, such as seizures, sudden confusion, or loss of consciousness.
People with pituitary disorders, recent head injury, chronic lung disease, or unexplained sodium abnormalities should not delay evaluation.
Sample Type
The ADH test is performed on a blood sample, usually drawn from a vein in the arm. To aid interpretation, urine samples and additional blood tests are often collected at the same time.
In selected cases, testing may be done under controlled hospital conditions to ensure reliable results.
Important Word Explanations
ADH (Antidiuretic Hormone): A hormone that regulates water balance by controlling urine output.
Vasopressin: Another name for antidiuretic hormone.
Osmolality: A measure of how concentrated blood or urine is.
Hyponatremia: Abnormally low sodium levels in the blood.
Reference Range: The expected normal limits of a laboratory test in healthy individuals.
People Also Ask
Is an ADH value outside the normal range always serious?
Not always. Mild changes can occur due to hydration, stress, or illness and need clinical correlation.
Can ADH levels change temporarily?
Yes. Fluid intake, pain, stress, and medications can cause short-term fluctuations.
Does an abnormal ADH result always mean a hormone disorder?
No. Sometimes the hormone level is normal, but the kidneys do not respond properly.
When do doctors usually worry about ADH levels?
When abnormal values are associated with symptoms or significant sodium imbalance.
Is repeat testing common for ADH?
Yes. Repeat or supportive tests are often needed for accurate interpretation.
Can a normal ADH level still cause symptoms?
Yes. If kidney response is impaired, symptoms can occur even with normal hormone levels.
~END~