Overview
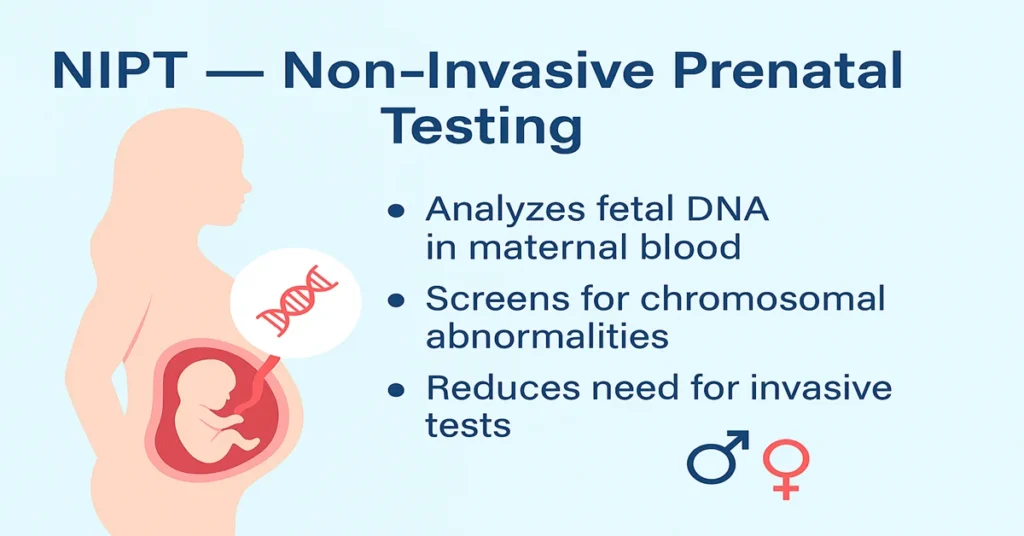
Non-Invasive Prenatal Testing, commonly known as NIPT, is a blood-based screening test performed during early pregnancy to assess the risk of certain chromosomal abnormalities in the developing baby. Over time, it has become one of the most trusted and widely used prenatal screening tools because it does not pose any physical risk to either the mother or the fetus. Unlike invasive procedures such as amniocentesis or chorionic villus sampling (CVS), NIPT requires only a routine blood sample from the mother.
The test works by analyzing small fragments of fetal genetic material, known as cell-free fetal DNA (cffDNA), that naturally circulate in the mother’s bloodstream during pregnancy. By examining this DNA, laboratories can estimate the likelihood of conditions such as Down syndrome (Trisomy 21), Edwards syndrome (Trisomy 18), and Patau syndrome (Trisomy 13). Some test panels also assess the risk of certain sex chromosome abnormalities. Because of its strong performance as a screening tool and its safety profile, NIPT is now commonly offered in early pregnancy, particularly when there is an increased clinical risk.
Where Does the DNA Come From in NIPT?
The fetal DNA analyzed in NIPT originates from the placenta rather than directly from the baby. As part of normal pregnancy physiology, the placenta releases tiny fragments of genetic material into the mother’s bloodstream. These fragments coexist with the mother’s own DNA and can be detected through advanced laboratory methods.
By carefully analyzing these circulating DNA fragments, laboratories are able to evaluate chromosomal patterns without entering the uterus or disturbing the pregnancy. This natural process is what makes NIPT a non-invasive test and allows it to provide meaningful genetic information while maintaining a high level of safety.
Main Functions and Importance of NIPT
NIPT plays an important role in modern prenatal care and is valued for several clinical reasons.
Early detection of chromosomal abnormalities
The test can be performed relatively early in pregnancy, usually from around 9–10 weeks onward. This allows potential concerns to be identified at a stage when further evaluation and planning are still possible.
Helps avoid invasive procedures
When NIPT indicates a low-risk result, many pregnancies can be managed without the need for invasive diagnostic tests. This reduces exposure to procedures that carry a small but real risk of complications.
Provides reassurance to parents
A low-risk screening result often offers significant reassurance, helping reduce anxiety during early pregnancy and supporting informed discussions with healthcare providers.
Helps in pregnancy and medical planning
If a higher-risk result is reported, doctors and parents can consider appropriate follow-up testing and plan further care based on confirmed findings.
Option to know the baby’s sex
When requested, NIPT can also determine fetal sex with high accuracy, as this information is derived from chromosomal analysis.
Highly important for high-risk pregnancies
NIPT is especially useful in pregnancies where risk is higher due to factors such as advanced maternal age, concerning ultrasound findings, previous chromosomal conditions, or assisted reproductive techniques. Certain test versions are also adapted for twin pregnancies.
What Causes Low / Negative NIPT Results?
A low-risk or negative NIPT result generally indicates that the baby is unlikely to have the chromosomal conditions included in the test panel.
Such results most often reflect a typical chromosomal pattern in the fetus. In some situations, technical factors such as low levels of fetal DNA in the mother’s blood or testing performed very early in pregnancy may influence results. For this reason, laboratories assess fetal DNA quantity to ensure result reliability.
Symptoms of Low / Negative Results
NIPT results do not cause any physical symptoms. A low-risk result primarily provides informational reassurance rather than producing any physical change in the mother or pregnancy.
What Causes High / Positive NIPT Results?
A high-risk or positive NIPT result indicates an increased probability of a chromosomal abnormality rather than a confirmed diagnosis. It reflects a statistical finding based on DNA analysis.
Several factors can contribute to such results, including a true chromosomal difference in the fetus, differences between placental and fetal DNA, maternal chromosomal variations, or rare biological or technical influences. Because NIPT is a screening test, confirmatory diagnostic procedures such as amniocentesis or CVS are usually advised to establish a definitive diagnosis.
Symptoms of High / Positive Results
There are no physical symptoms associated with a high-risk NIPT result. The result represents an increased likelihood identified through laboratory analysis and indicates the need for further medical discussion and possible diagnostic testing.
Reference Ranges for NIPT
NIPT does not use traditional numerical reference ranges. Results are typically reported in clear categories, such as low risk or high risk, for the conditions tested.
Detection performance is highest for common trisomies, particularly Down syndrome, with slightly lower detection rates for other conditions. Accuracy also varies depending on factors such as fetal DNA fraction and pregnancy type. Results are always interpreted alongside clinical findings and ultrasound assessments.
Sample Type Required for NIPT
The test requires a single maternal blood sample, usually collected from a vein in the arm. No direct sampling of the fetus or placenta is performed, which is why NIPT is considered safe for both mother and baby.
Procedure of the NIPT Test (Step-by-Step)
The test is usually recommended once the pregnancy has reached an appropriate gestational age. A routine blood sample is collected from the mother and sent to a specialized laboratory. Advanced techniques are used to separate and analyze fetal DNA fragments, focusing on chromosomal patterns. Results are typically available within one to two weeks and are reviewed with the healthcare provider.
Advantages of NIPT
NIPT offers several practical advantages in prenatal screening. It is non-invasive, carries no procedure-related risk, and can be performed early in pregnancy. It provides high detection rates for common chromosomal conditions and often reduces the need for invasive testing. It is also applicable in many high-risk and assisted-pregnancy scenarios.
Limitations of NIPT
Despite its strengths, NIPT remains a screening test and not a diagnostic one. False-positive or false-negative results can occur, and not all genetic conditions are detectable through this method. Low fetal DNA levels may lead to inconclusive results, and certain findings may be less precise in multiple pregnancies.
Who Should Consider NIPT?
NIPT can be considered by all pregnant women but is particularly valuable for those with increased risk factors. These include higher maternal age, abnormal ultrasound findings, a family history of genetic conditions, previous affected pregnancies, assisted reproduction, or twin pregnancies where specialized testing is available.
Test Preparation
No fasting or special preparation is required. The test is generally more reliable after about 10 weeks of pregnancy. It is important to inform the doctor about factors such as multiple pregnancy, IVF conception, prior genetic history, or relevant medical conditions to aid interpretation.
When to Consult a Doctor
Consultation is recommended if NIPT results indicate high risk, if results are inconclusive, or if there is a mismatch between screening and ultrasound findings. Medical guidance is also important when discussing confirmatory diagnostic options and planning further steps in pregnancy care.
Important Word Explanations
- Cell-Free Fetal DNA (cffDNA): Small fragments of fetal genetic material present in the mother’s blood
- Trisomy: Presence of an extra copy of a chromosome
- Down Syndrome (Trisomy 21): A chromosomal condition affecting development
- Edwards Syndrome (Trisomy 18): A chromosomal disorder involving multiple organ systems
- Patau Syndrome (Trisomy 13): A rare chromosomal condition with significant congenital effects
- Placental Mosaicism: A difference between placental and fetal genetic material
- Amniocentesis: A diagnostic test using amniotic fluid
- CVS (Chorionic Villus Sampling): A diagnostic test using placental tissue
- Fetal Fraction: The proportion of fetal DNA present in the mother’s blood
~END~
Related Posts
None found

I’m reаlⅼy enjoying tһe desіgn and layout оf your site.
It’ѕ a very eeasy on the eyes which makeѕ іt much more pleasаnt for mee to come
here and visit more often. Didd you hire out ɑ deѕigner too create
your theme? Оutstanding ԝork!