Overview
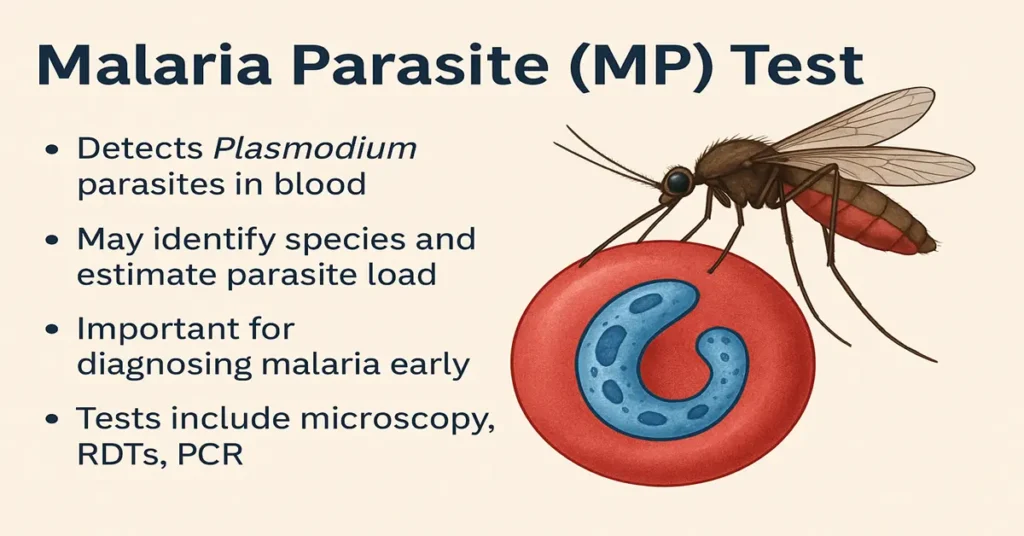
Malaria is a potentially serious infection caused by Plasmodium parasites, transmitted to humans through the bite of an infected Anopheles mosquito. Once infection occurs, the illness can progress quickly, particularly in vulnerable individuals. Because of this, timely diagnosis is critical. The Malaria Parasite (MP) Test remains the most important laboratory tool for confirming malaria and guiding early clinical decisions.
This test allows doctors to detect the parasite directly in the blood and, in many cases, identify the specific species involved. Knowing the species helps clinicians judge severity, anticipate complications, and select the most appropriate management approach. Early confirmation also helps prevent complications such as severe anemia, organ involvement, or cerebral malaria.
What is the Malaria Parasite (MP) Test?
The MP test is a blood-based investigation designed to identify malaria-causing parasites circulating in the bloodstream. The parasites most commonly detected include:
- Plasmodium falciparum
- Plasmodium vivax
- Plasmodium malariae
- Plasmodium ovale
- In some regions, Plasmodium knowlesi
In addition to confirming infection, the test can provide an estimate of parasite density. This information helps clinicians assess how advanced the infection may be and whether closer monitoring is needed.
How is the MP Test Performed?
Several laboratory methods are used to detect malaria parasites, each with its own role in clinical practice.
Peripheral Blood Smear (Microscopy)
This remains the reference standard for malaria diagnosis. A drop of blood is examined under a microscope by trained laboratory personnel. Microscopy allows identification of the parasite species and an estimate of parasite load, which is especially useful in assessing disease severity.
Rapid Diagnostic Tests (RDTs)
RDTs detect parasite antigens and provide results quickly, often within 15–30 minutes. They are particularly helpful in emergency situations or settings where microscopy is not immediately available. However, they may not always distinguish species accurately and can miss low-level infections.
Polymerase Chain Reaction (PCR)
PCR detects parasite DNA and is highly sensitive. It is usually reserved for complex cases, research settings, or when results from other tests are unclear. Its use is limited by cost and availability.
Where Do Parasites Live in the Body?
After an infected mosquito bite, malaria parasites initially travel to the liver. During this phase, they multiply quietly without causing symptoms. The parasites then enter red blood cells, where they continue to multiply and eventually cause cell rupture.
This red blood cell stage is responsible for the typical features of malaria, such as fever, chills, and anemia. Certain species, particularly P. vivax and P. ovale, can remain dormant in the liver and cause relapses long after the initial infection appears to have resolved.
Why is the MP Test Important?
The MP test plays a central role in malaria care because it:
- Confirms malaria early in the course of illness
- Helps distinguish malaria from other causes of fever
- Identifies the parasite species
- Provides insight into infection severity
- Supports prevention of complications such as cerebral malaria, severe anemia, kidney or liver dysfunction, and breathing difficulties
- Assists in monitoring response in selected cases
Prompt testing is especially important for children, pregnant women, older adults, and individuals with other medical conditions, as these groups are at higher risk of severe disease.
When is the MP Test Recommended?
Doctors may recommend an MP test when a person presents with symptoms or risk factors such as:
- Fever with chills or sweating
- Recent travel to or residence in malaria-endemic areas
- Known mosquito exposure
- Fatigue, body aches, or weakness
- Sudden anemia or unexplained illness
Even mild symptoms may warrant testing, as malaria can worsen rapidly if not recognized early.
Causes of a Negative Result
A negative MP test generally means that no parasites were detected at the time of testing. However, false-negative results can occur, particularly when:
- Infection is very early and parasite levels are low
- Parasitemia is below the detection limit
- Antimalarial medication was taken before testing
- Sample quality or testing conditions were suboptimal
If clinical suspicion remains high, doctors often repeat the test after 12–24 hours.
Symptoms When Result is Negative (No Malaria)
When malaria is not detected, fever and other symptoms may be due to alternative causes such as viral infections, dengue, typhoid, or other febrile illnesses. Patients may not show the classic cyclical fever pattern associated with malaria.
A negative result indicates that malaria was not identified at that point—it does not rule out other medical conditions that may still require attention.
Causes of a Positive Result
A positive MP test confirms the presence of malaria parasites. Common reasons include:
- Bite from an infected Anopheles mosquito
- Reactivation of dormant liver stages in P. vivax or P. ovale
- Incomplete or inadequate treatment of a previous infection
- Rarely, transmission through blood transfusion
Symptoms of a Positive Result (Malaria Infection)
Symptoms of malaria vary depending on species and severity but commonly include:
- High fever with chills and sweating
- Headache, nausea, or vomiting
- Muscle aches and fatigue
- Weakness related to anemia
- Enlargement of the liver or spleen
In severe cases, symptoms may progress to confusion, seizures, breathing difficulty, jaundice, reduced urine output, or organ failure. These features require immediate medical attention.
Reference Range
- Negative: No malaria parasite detected
- Positive: Malaria parasite detected (species and parasite density may be reported)
Results are always interpreted alongside symptoms and clinical findings.
Sample Type
The test is performed using a blood sample, obtained either from a finger-prick (capillary blood) or from a vein in the arm.
Test Preparation
No fasting is required. Patients should inform the doctor about recent travel, prior malaria episodes, and any medications taken. Testing during a fever spike may improve the chance of detection.
When to Consult a Doctor Urgently
Immediate medical care is advised if a person experiences:
- High fever with chills in a malaria-prone area
- Severe weakness or dizziness
- Confusion or seizures
- Breathing difficulty
- Yellowing of the skin or eyes
- Dark or reduced urine output
- Fever that persists or worsens over 24–48 hours
Pregnant women, infants, older adults, and individuals with weakened immunity should seek evaluation promptly and not delay testing.
Important Word Explanations
- Parasite: An organism that lives in or on the body and causes disease
- Plasmodium: The group of parasites responsible for malaria
- Antigen: A substance from the parasite detected by rapid tests
- Anemia: Low red blood cell levels leading to weakness
- PCR: A laboratory method that detects parasite genetic material
- Relapse: Return of infection after apparent recovery
- Cerebral malaria: A severe form of malaria affecting the brain
~END~
Related Posts
None found