Causes and Symptoms of Low Alpha-1 Antitrypsin (A1AT) Levels
Overview of Low Levels
Alpha-1 Antitrypsin (A1AT) is a protective protein made mainly in the liver and released into the bloodstream. In routine clinical terms, its job is simple but crucial: it protects tissues—especially the lungs—from damage caused by enzymes released during inflammation. When A1AT levels are adequate, this protection works quietly in the background. When levels are low, the balance shifts, and normal tissues can slowly get damaged.
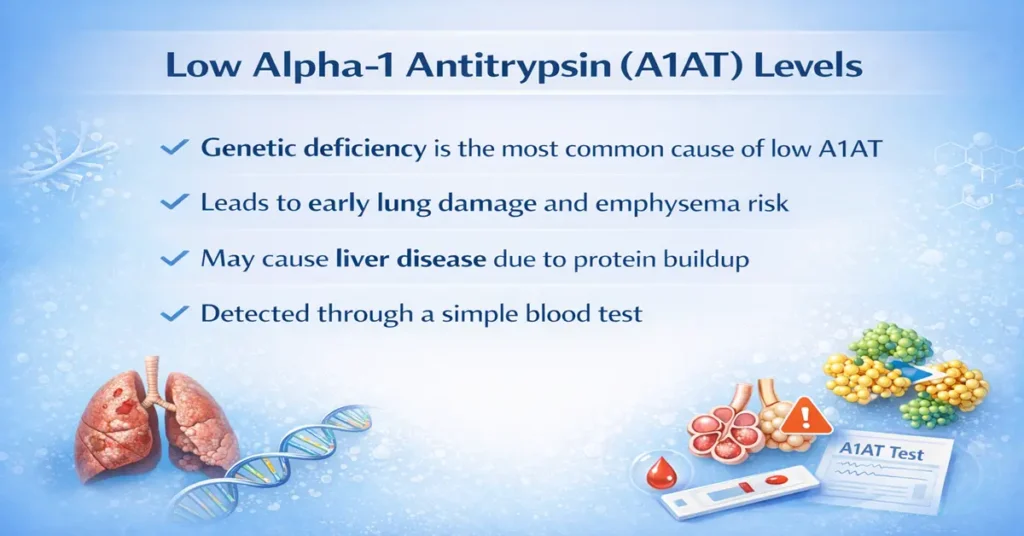
Low A1AT levels are most commonly linked to Alpha-1 Antitrypsin Deficiency, a genetic condition. Many individuals with low levels feel well for years, which is why the condition often goes undetected until lung or liver problems appear. Understanding why A1AT is low and how it shows up clinically helps prevent long-term complications.
Major Medical Causes of Low A1AT Levels
The most frequent cause of low A1AT levels is an inherited change in the SERPINA1 gene. This gene controls how A1AT is made and released into the blood.
In Alpha-1 Antitrypsin Deficiency, the liver produces an abnormal form of the protein. This abnormal A1AT cannot be released efficiently into the bloodstream, so blood levels remain low while the protein accumulates inside liver cells.
Advanced liver disease can also lower A1AT levels. Because the liver is responsible for producing A1AT, severe damage—such as cirrhosis or long-standing hepatitis—can reduce production.
Less commonly, protein-losing conditions may be involved. Disorders like nephrotic syndrome or severe intestinal disease can cause loss of proteins from the body, including A1AT, leading to reduced measured levels in blood tests.
Symptoms Seen in Low A1AT Levels
Symptoms depend on how low the A1AT level is and which organs are affected. Some people remain symptom-free for a long time, while others develop problems earlier.
In adults, lung-related symptoms are most common. These include shortness of breath, wheezing, chronic cough, frequent chest infections, and reduced exercise tolerance. Clinically, many patients are first labeled as having asthma or COPD, especially if symptoms appear earlier than expected.
Liver involvement may present as fatigue, yellowing of the skin or eyes, abdominal swelling, easy bruising, or persistently abnormal liver enzymes on blood tests.
In infants and children, low A1AT levels can show up as prolonged jaundice, poor weight gain, enlarged liver, or pale stools. These signs often trigger early testing and diagnosis.
Health Risks of Persistently Low Levels
Persistently low A1AT levels can lead to progressive lung damage. Without adequate protection, lung tissue becomes vulnerable to enzyme-related injury, increasing the risk of early-onset emphysema—even in people who have never smoked. Smoking, however, dramatically accelerates lung damage and worsens outcomes.
Chronic liver disease is another major concern. Accumulation of abnormal A1AT protein inside liver cells can cause inflammation, fibrosis, cirrhosis, and in some cases liver failure or liver cancer.
Low A1AT levels have also been linked, though less commonly, to conditions such as panniculitis, a painful inflammatory skin disorder, and certain forms of vasculitis.
From real-world practice, outcomes are significantly better when the condition is identified early and managed appropriately.
How to Improve Levels Safely
Low Alpha-1 Antitrypsin levels cannot be reliably increased naturally at home, as the condition is usually genetic. Attempts to “boost” levels without medical guidance are ineffective and unsafe. Management focuses on protection and medical treatment rather than direct correction.
In selected patients, A1AT augmentation therapy may be used. This involves intravenous infusion of purified A1AT to raise blood levels and protect lung tissue. It is prescribed only after careful evaluation and is not suitable for everyone.
Avoiding lung irritants is critical. Complete avoidance of smoking and second-hand smoke is the single most important protective step. Occupational exposure to dust, fumes, and chemicals should also be minimized.
Vaccinations against influenza, pneumonia, and hepatitis help reduce infections that can worsen lung and liver damage. Regular monitoring of lung function and liver enzymes allows early detection of complications.
Healthy nutrition, weight control, and limiting alcohol help protect the liver, even though these measures do not directly increase A1AT levels.
Additional Information
Low A1AT levels are often underdiagnosed because symptoms overlap with common lung and liver conditions. Once a diagnosis is confirmed, family screening is strongly advised, as close relatives may carry the same genetic change.
Genetic counseling helps patients understand inheritance patterns and future risks. Early awareness allows preventive care long before serious damage develops.
Test Preparation
The A1AT blood test usually requires no special preparation. Fasting is not needed unless other tests are ordered at the same time. Patients should inform their doctor about recent infections or inflammation, as these can temporarily raise A1AT levels and affect interpretation.
When to See a Doctor
Medical advice should be sought if there is unexplained shortness of breath, early-onset COPD, persistently abnormal liver enzymes, prolonged jaundice in infants, or a strong family history of lung or liver disease. Early testing helps prevent irreversible complications.
Sample Type
The A1AT test is performed using a blood sample, typically drawn from a vein in the arm. Genetic testing may also be done using blood or saliva to confirm inherited deficiency.
Important Word Explanations
Alpha-1 Antitrypsin (A1AT): A protective protein that prevents enzyme-related tissue damage, mainly in the lungs
Alpha-1 Antitrypsin Deficiency: A genetic condition that causes low A1AT levels
Emphysema: A lung disease where air sacs are damaged, leading to breathing difficulty
Augmentation Therapy: Medical treatment that replaces missing A1AT protein
Cirrhosis: Long-term scarring of the liver due to chronic damage
People Also Ask
Is a low A1AT level always serious?
Not always immediately, but persistently low levels increase the risk of lung and liver disease over time.
Can low A1AT levels be temporary?
Usually no. Most low levels are genetic, though test values can vary slightly with illness or inflammation.
Does low A1AT always mean lung disease?
No. Some people have low levels without symptoms, especially early in life.
When do doctors usually worry about low A1AT?
When low levels are combined with early breathing problems, liver abnormalities, or a strong family history.
Is repeat testing common for A1AT?
Yes. Repeat blood tests and genetic confirmation are often done to be sure of the diagnosis.
Should family members be tested if A1AT is low?
Yes. Family screening is recommended because the condition is inherited.
~END~