Causes and Symptoms of Low Aldosterone Levels
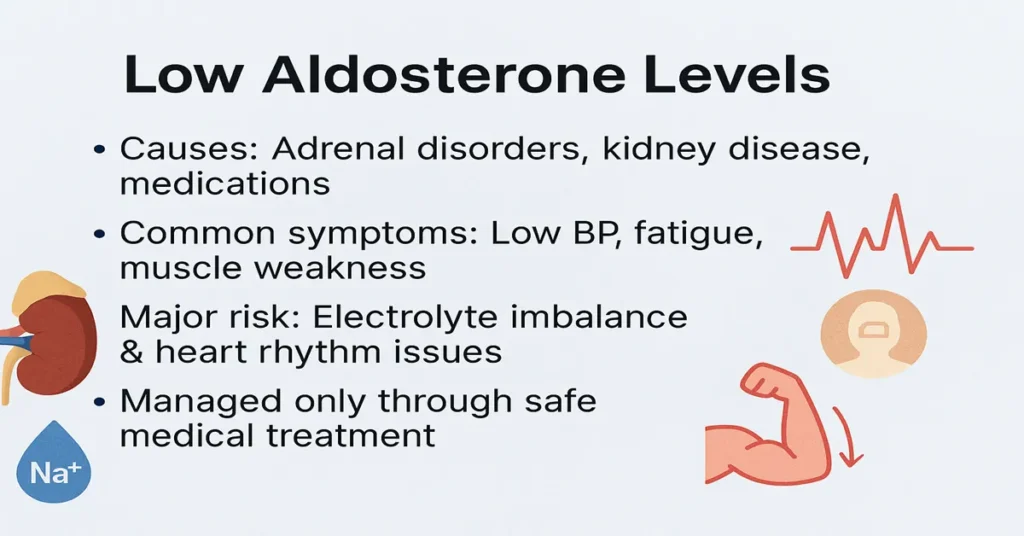
Low aldosterone levels are an important medical finding because aldosterone is a key hormone that helps regulate blood pressure, fluid balance, and electrolyte levels in the body. When aldosterone levels fall below normal, the body struggles to hold on to sodium and water while clearing excess potassium. Over time, this imbalance can affect the heart, muscles, kidneys, and overall circulation.
This article explains low aldosterone levels in a practical, clinical way—covering causes, symptoms, risks, and how doctors usually approach management. Because aldosterone is a hormone, it cannot be safely corrected at home, and treatment decisions must always be guided by medical evaluation.
Overview of Low Aldosterone Levels
Aldosterone is produced by the adrenal glands, which sit just above the kidneys. Its main job is to signal the kidneys to retain sodium and water and to excrete potassium. This action helps maintain normal blood volume and stable blood pressure.
Low aldosterone levels, medically called hypoaldosteronism, occur when the adrenal glands produce too little aldosterone or when the kidneys do not respond properly to it. As a result, sodium and water are lost in urine, potassium builds up in the blood, and blood pressure may fall.
Clinically, this hormone imbalance often shows up through symptoms rather than lab values alone. Doctors usually look for patterns—low blood pressure, electrolyte changes, and related hormone results—before drawing conclusions.
Major Medical Causes of Low Aldosterone Levels
Several conditions can reduce aldosterone production or interfere with how it works in the body.
Adrenal gland disorders
Damage or dysfunction of the adrenal glands is a common cause. Conditions such as adrenal insufficiency can reduce aldosterone production along with other adrenal hormones.
Congenital adrenal conditions
Some individuals are born with genetic disorders that affect adrenal hormone synthesis. In these cases, low aldosterone may be present from childhood and requires long-term medical care.
Kidney-related causes
Sometimes aldosterone production is normal, but the kidneys do not respond as expected. This is seen in hyporeninemic hypoaldosteronism, often associated with chronic kidney disease or long-standing diabetes.
Medications
Certain drugs can suppress aldosterone or block its effects. These include some blood pressure medicines, potassium-sparing diuretics, and medications that act on the renin–angiotensin system. In routine practice, medication review is a key step when low aldosterone is detected.
Severe illness or stress
Serious infections, trauma, or prolonged illness can temporarily reduce adrenal hormone output. In these situations, low aldosterone may improve once the underlying stress resolves.
Identifying the exact cause is essential because management depends on correcting the underlying problem, not just the hormone level.
Symptoms Seen in Low Aldosterone Levels
Symptoms usually develop gradually and can be subtle at first. Many patients do not realize their symptoms are hormone-related until testing is done.
Common symptoms include persistent fatigue, generalized weakness, dizziness (especially on standing), and low blood pressure. Salt craving is a frequent complaint and is often a clue clinicians take seriously.
Because aldosterone helps regulate potassium, higher potassium levels may develop and lead to muscle heaviness, cramps, tingling sensations, or irregular heartbeats. Some people notice frequent urination or signs of dehydration despite adequate fluid intake.
The severity of symptoms depends on how low aldosterone levels are and whether other adrenal hormones, such as cortisol, are also affected.
Health Risks of Persistently Low Aldosterone Levels
If low aldosterone levels are not addressed, ongoing electrolyte and fluid imbalance can lead to important health risks.
Chronic low blood pressure increases the risk of dizziness, fainting, and falls. Persistently abnormal sodium and potassium levels can interfere with heart rhythm and nerve function, which may become dangerous if left untreated.
In people with kidney disease, electrolyte imbalance adds further strain and can worsen kidney function. When low aldosterone occurs as part of adrenal insufficiency, the risk of adrenal crisis increases, especially during illness or physical stress. This is a medical emergency that requires immediate care.
Early diagnosis and proper medical management greatly reduce these risks.
How to Improve Aldosterone Levels Safely
Aldosterone is not a vitamin or nutrient that can be safely boosted at home. There are no reliable natural methods to raise aldosterone levels without medical supervision.
Management focuses on treating the underlying cause. If an adrenal or kidney disorder is responsible, that condition is addressed directly. In some cases, doctors prescribe mineralocorticoid replacement medicines that mimic aldosterone’s effects in the body, helping normalize sodium, potassium, and blood pressure.
Doctors may also adjust fluid or salt intake based on test results, symptoms, and overall health. If medications are contributing, treatment plans are reviewed and adjusted where appropriate.
Self-treatment, hormone use without prescription, or unsupervised salt loading can be harmful and should be avoided.
Additional Information
Low aldosterone levels are usually evaluated alongside related hormones such as renin and cortisol. Looking at these together helps doctors determine whether the problem lies in the adrenal glands, kidneys, or hormonal control system.
In many patients, symptoms improve significantly once the correct diagnosis is made and appropriate treatment begins. Some conditions require long-term follow-up, while others resolve once the underlying cause is corrected.
Test Preparation
Proper preparation is important for accurate aldosterone testing. Patients may be advised to follow specific instructions regarding salt intake, posture, and timing of the test, as aldosterone levels vary during the day.
It is essential to inform the doctor about all medications and supplements, as many can affect results. Always follow the laboratory or doctor’s instructions closely.
When to See a Doctor
You should consult a doctor if you experience persistent dizziness, unexplained fatigue, muscle cramps, irregular heartbeat, or consistently low blood pressure. Medical evaluation is especially important if aldosterone test results are abnormal or if you have known adrenal or kidney disease.
Early assessment helps prevent complications and allows timely, effective treatment.
Sample Type
Aldosterone testing is usually done using a blood sample drawn from a vein in the arm. In some cases, a urine test may also be used to assess aldosterone levels over a longer period.
Important Word Explanations
Aldosterone: A hormone produced by the adrenal glands that regulates sodium, potassium, and blood pressure.
Adrenal Glands: Small glands above the kidneys that produce essential hormones.
Electrolytes: Minerals such as sodium and potassium that control nerve, muscle, and heart function.
Hypoaldosteronism: A condition in which the body produces too little aldosterone.
Hormone Replacement Therapy: Medical treatment used to replace deficient hormones.
People Also Ask
Is low aldosterone a serious condition?
It can be serious if untreated, especially when it causes electrolyte imbalance or low blood pressure, but many cases are manageable with proper care.
Can low aldosterone levels be temporary?
Yes. Severe illness, stress, or certain medications can cause temporary suppression that improves once the trigger resolves.
Does low aldosterone always mean adrenal disease?
No. Kidney-related causes and medication effects are also common and must be evaluated.
When do doctors usually worry about low aldosterone?
When symptoms are present, potassium is high, blood pressure is low, or results persist on repeat testing.
Is repeat testing common?
Yes. Repeat tests help confirm results and understand hormone patterns over time.
Can symptoms improve after treatment?
In most cases, symptoms improve significantly once the underlying cause is identified and managed properly.
~END~