Japanese Encephalitis (JEV) Antibody Test: Purpose, IgM/IgG Meaning, High-Low Levels & Diagnosis Guide
Overview
Japanese Encephalitis (JE) is a mosquito-borne viral infection that affects the central nervous system, particularly the brain. It is seen mainly in rural and agricultural regions of Asia, especially areas with rice cultivation. Most people infected with the Japanese Encephalitis Virus (JEV) never develop noticeable illness. However, in a small proportion of cases, the virus can cause inflammation of the brain (encephalitis), which may lead to serious neurological complications.
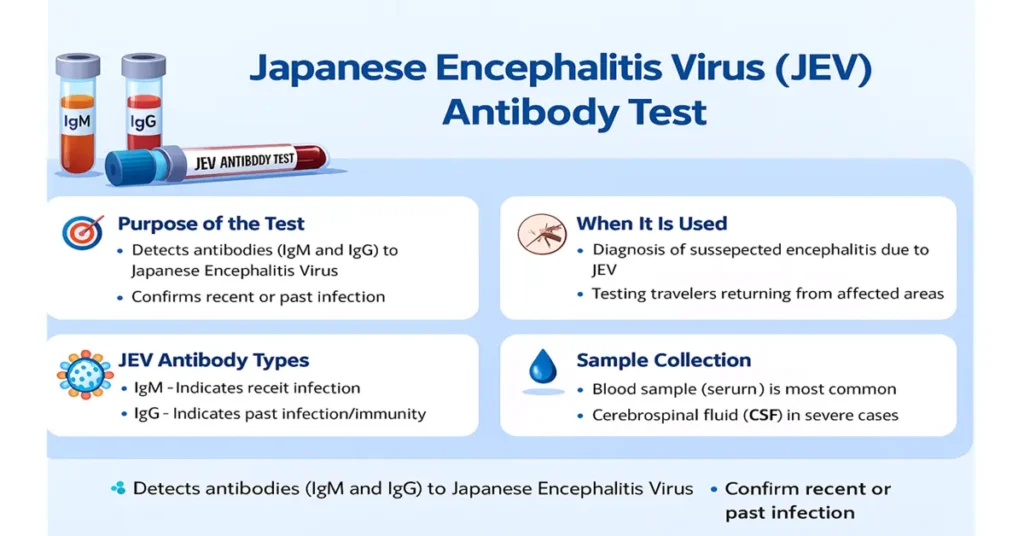
Because the early symptoms often resemble other common infections, clinical examination alone is usually not enough to confirm JE. This is where the JEV Antibody Test becomes important. By detecting specific antibodies produced by the immune system, the test helps doctors determine whether JEV infection is recent, occurred in the past, or reflects immunity from vaccination. It is particularly useful during outbreaks, in travelers returning from endemic regions, and in patients presenting with signs of brain involvement.
What Is the JEV Antibody Test?
The JEV Antibody Test is a blood-based laboratory test that measures the body’s immune response to the virus. It mainly looks for two types of antibodies: IgM and IgG.
IgM antibodies usually appear first, within days to weeks after infection, and are considered a marker of recent or ongoing infection. IgG antibodies develop later and tend to persist for a long time, indicating past infection or immunity, often from vaccination.
From a practical clinical standpoint, IgM positivity raises concern for a recent infection, while IgG positivity alone usually reflects past exposure or immune memory. Doctors rely on this antibody pattern to confirm suspected JE, distinguish new infections from old ones, assess immune status in vaccinated individuals, and support diagnosis in patients with unexplained brain inflammation. In acute settings, especially when neurological symptoms are present, these results help guide further evaluation and monitoring.
Where Are JEV Antibodies Produced?
JEV antibodies are produced by the body’s immune system rather than by the virus itself. After the virus enters the body—most commonly through a mosquito bite, or less commonly following vaccination—the immune system recognizes it as foreign.
Specialized immune cells known as B lymphocytes become activated and mature into plasma cells. These plasma cells release IgM antibodies during the early phase of exposure and IgG antibodies later on, which provide longer-term immune memory. This antibody production is a normal protective response and forms the basis of laboratory testing for JEV.
Why Is the JEV Antibody Test Important?
The value of the JEV Antibody Test lies in its ability to bring clarity to complex clinical situations. Symptoms of JE can closely resemble those of dengue, malaria, meningitis, or other viral infections. Antibody detection helps identify JEV as the cause when the clinical picture is unclear.
The test also allows doctors to distinguish between a recent infection and a past exposure by comparing IgM and IgG results. In patients with encephalitis, seizures, or altered mental status, detection of JEV antibodies—especially in cerebrospinal fluid—adds strong diagnostic support. During outbreaks, these results assist public health teams in tracking disease spread, while IgG testing helps confirm immune response following vaccination. Overall, timely and accurate antibody testing plays a key role in patient evaluation and disease surveillance.
Causes of Low or Negative JEV Antibody Results
A low or negative antibody result most often means there has been no exposure to the virus. In some cases, testing may have been done very early, before the immune system has had enough time to produce detectable antibodies. This can lead to a temporary false-negative result.
In individuals with reduced immune responses, such as very young children, elderly patients, or those with immune suppression, antibody production may be lower than expected. Rarely, technical factors in the laboratory can also affect results. For these reasons, results are always interpreted in the context of symptoms, timing, and clinical findings.
Symptoms When Antibodies Are Low or Negative
Low or negative antibody levels do not cause symptoms by themselves. If a patient has symptoms suggestive of JE—such as fever, headache, vomiting, confusion, or seizures—but antibody results are negative, doctors may consider repeat testing after a short interval or evaluate cerebrospinal fluid. This approach reflects clinical caution rather than a definitive exclusion of disease.
Causes of High or Positive JEV Antibody Results
A positive antibody result can have several interpretations. IgM positivity usually indicates a recent infection and suggests that the virus has triggered an active immune response. IgG positivity alone generally reflects past infection or immunity following vaccination.
In regions where other flaviviruses are common, cross-reactivity can occur. Viruses such as dengue, West Nile virus, or Zika share structural similarities with JEV, and this can occasionally lead to false-positive results. For this reason, doctors consider exposure history, symptoms, and, when needed, additional confirmatory tests.
Symptoms Linked to High or Positive Results
When IgM antibodies are positive, patients may show signs consistent with acute infection, including fever, severe headache, vomiting, confusion, seizures, weakness, or reduced consciousness. These findings suggest active brain involvement and require urgent medical evaluation.
Isolated IgG positivity, on the other hand, is usually not associated with symptoms. It indicates previous exposure or immunity and does not suggest active disease on its own.
Reference Ranges
JEV antibody results are commonly reported as negative, equivocal, or positive. IgM positivity supports recent infection, while IgG positivity indicates past infection or immunity. Exact cutoff values depend on the testing method used, such as ELISA or other immunoassays, and are interpreted by the laboratory in conjunction with clinical information.
Sample Type
The test is most commonly performed on a blood (serum) sample. In patients with neurological symptoms, cerebrospinal fluid may also be tested. Detection of IgM antibodies in CSF is considered highly suggestive of central nervous system involvement by JEV.
Test Preparation
No special preparation is required for this test. Fasting and dietary changes are not needed. Doctors usually ask about recent travel, possible mosquito exposure, vaccination history, and current symptoms. In severe cases, testing may be done urgently as part of hospital evaluation.
When to Consult a Doctor
Medical attention is advised if symptoms such as persistent fever, severe headache, nausea, or vomiting develop, especially after travel to JE-affected areas. Neurological signs like confusion, seizures, difficulty speaking, weakness, or paralysis warrant immediate evaluation. Loss of consciousness, breathing difficulty, or severe seizures are emergency situations and require urgent care.
Important Word Explanations
- Encephalitis: Inflammation of the brain
- Antibodies: Protective proteins produced by the immune system
- IgM: Antibody indicating recent or active infection
- IgG: Antibody indicating past infection or immunity
- Flavivirus: A group of related viruses that includes JEV and dengue
- CSF: Cerebrospinal fluid surrounding the brain and spinal cord
~END~
Related Posts
None found