Intact Parathyroid Hormone (iPTH) Test: Role, High/Low Levels, Symptoms & Medical Guide
What Is Intact Parathyroid Hormone (iPTH)?
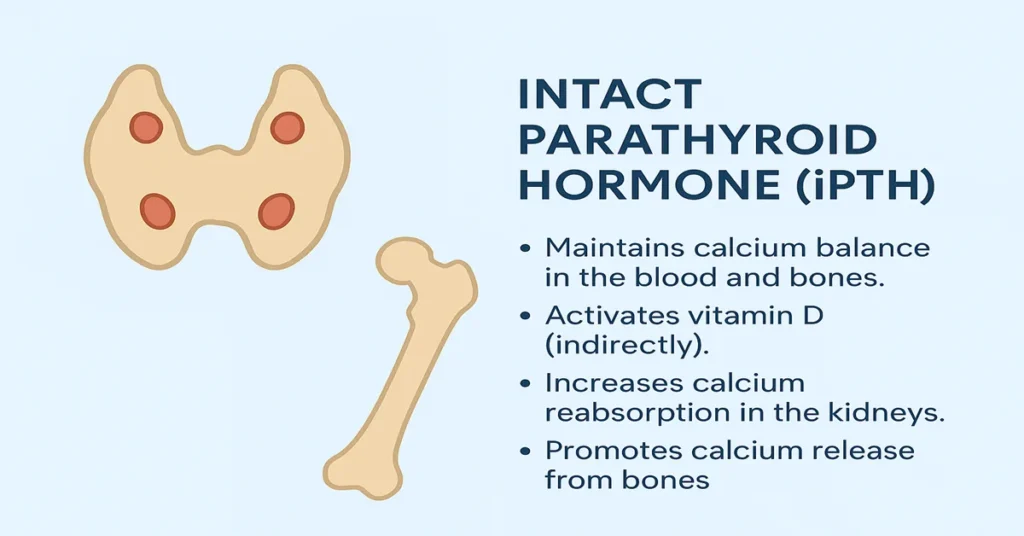
The Intact Parathyroid Hormone (iPTH) test measures the level of parathyroid hormone circulating in the blood. Parathyroid hormone plays a central role in maintaining the body’s calcium and phosphorus balance and in regulating vitamin D activity. These processes are essential for healthy bones, proper nerve signaling, normal muscle contraction, and stable kidney function.
Even small changes in PTH levels can affect calcium balance, which is why the iPTH test is commonly used when doctors are evaluating unexplained calcium abnormalities or suspected parathyroid disorders. Rather than being interpreted alone, iPTH is usually assessed alongside blood calcium, phosphorus, and vitamin D levels to provide a complete picture of mineral regulation.
Clinically, the test is often requested when doctors are considering conditions such as parathyroid overactivity or underactivity, vitamin D–related imbalance, kidney disease–associated bone disorders, or unexplained bone loss.
Where Is iPTH Produced in the Body?
Intact parathyroid hormone is produced exclusively by the parathyroid glands. These are small, pea-sized glands located behind the thyroid gland in the neck. Most individuals have four parathyroid glands, though natural variations are common.
The parathyroid glands continuously sense blood calcium levels. When calcium levels fall, PTH secretion increases to restore balance. When calcium levels rise, PTH release is suppressed. This constant feedback system helps maintain stable calcium levels throughout the day, allowing nerves, muscles, and bones to function normally.
Main Functions and Importance of iPTH
1. Maintains Blood Calcium Levels
The primary role of PTH is to prevent blood calcium from falling too low. Calcium is critical for muscle movement, heart rhythm stability, blood clotting, and nerve impulse transmission. When calcium levels begin to drop, PTH rises promptly to correct the imbalance.
2. Activates Vitamin D
PTH stimulates the kidneys to convert vitamin D into its active form, calcitriol. Active vitamin D improves calcium absorption from the intestines, helping maintain adequate calcium availability for the body’s needs.
3. Reduces Calcium Loss Through Kidneys
PTH signals the kidneys to conserve calcium by reducing its loss in urine. This mechanism becomes particularly important when dietary intake or absorption is insufficient.
4. Releases Stored Calcium From Bones
When blood calcium levels are low, PTH can trigger the release of calcium from bone stores. This helps stabilize blood levels but, if sustained over long periods, may gradually affect bone strength.
5. Controls Phosphorus Levels
PTH also influences phosphorus balance by increasing its excretion through the kidneys. Maintaining the correct calcium–phosphorus ratio is essential for proper bone mineralization and metabolic stability.
Together, these actions make iPTH a key regulator of bone health, neuromuscular function, and kidney-related mineral balance.
Causes of Low iPTH Levels
Low iPTH levels generally reflect reduced parathyroid gland activity and are often associated with low blood calcium.
1. Hypoparathyroidism
This is the most common clinical cause of low PTH. It may occur after thyroid or neck surgery, due to autoimmune processes, or from congenital absence or dysfunction of the parathyroid glands.
2. Low Magnesium Levels
Magnesium is required for normal PTH secretion. When magnesium levels are low, PTH release can be impaired even if the parathyroid glands themselves are structurally normal.
3. Vitamin D Excess
Very high vitamin D levels can suppress PTH production, as the body senses sufficient calcium availability.
4. Genetic or Chronic Calcium Disorders
Rare inherited or long-standing conditions affecting calcium regulation may also lead to reduced PTH levels.
Symptoms of Low iPTH Levels
Symptoms associated with low iPTH usually arise from low calcium levels rather than the hormone deficiency itself. These may include muscle cramps, tingling sensations in the lips or extremities, muscle stiffness, or spasms. In more pronounced cases, seizures or significant neuromuscular irritability can occur.
Additional features such as fatigue, mood changes, dry skin, brittle nails, or hair changes may be observed over time. The severity of symptoms depends on how low calcium levels are and how rapidly they have fallen.
Causes of High iPTH Levels
Elevated iPTH levels can reflect primary parathyroid disorders or secondary responses to other medical conditions.
1. Primary Hyperparathyroidism
This condition occurs when one or more parathyroid glands become overactive, often due to a benign adenoma or gland enlargement. In this setting, both calcium and PTH levels are typically elevated.
2. Secondary Hyperparathyroidism
Secondary hyperparathyroidism is a compensatory response, most commonly seen in chronic kidney disease, vitamin D deficiency, calcium deficiency, or malabsorption states. Here, PTH rises in response to low or poorly utilized calcium.
3. Tertiary Hyperparathyroidism
In long-standing kidney disease, prolonged stimulation of the parathyroid glands may lead to persistent overactivity. In this stage, PTH levels remain high even if calcium levels begin to normalize.
4. Gastrointestinal Malabsorption
Conditions that impair nutrient absorption can reduce calcium and vitamin D availability, prompting increased PTH secretion as a compensatory mechanism.
Symptoms of High iPTH Levels
Symptoms related to high PTH vary depending on the underlying cause and the associated calcium level. Bone-related effects may include bone discomfort, reduced bone density, or increased fracture risk over time. Kidney-related effects can include kidney stones or increased urine output.
Digestive complaints such as abdominal discomfort or constipation may occur when calcium levels are elevated. General symptoms can include fatigue, muscle weakness, mood changes, or cognitive slowing. In more severe cases of high calcium, confusion or marked weakness may be observed.
Reference Ranges
Typical reference values for iPTH vary by laboratory, but a commonly used adult range is approximately 10–65 pg/mL.
Interpretation should always take into account calcium, phosphorus, vitamin D status, and kidney function. An isolated PTH value is rarely sufficient for diagnosis without these accompanying measurements.
Sample Type
The iPTH test is performed using a blood sample, collected as serum or plasma. Some laboratories prefer EDTA tubes based on their testing method.
Test Preparation
Fasting is usually not required. Doctors may consider recent calcium or vitamin D supplementation, kidney-related medications, or biotin use when interpreting results, as these can influence laboratory measurements.
When to Consult a Doctor
Medical evaluation is recommended if symptoms suggest calcium imbalance. These include tingling sensations, muscle cramps, spasms, seizures, excessive thirst, frequent urination, bone pain, or symptoms suggestive of kidney stones.
Regular monitoring is also important for individuals with chronic kidney disease, those who have undergone thyroid or neck surgery, or patients with known parathyroid disorders. Abnormal iPTH results are typically assessed by an endocrinologist or nephrologist, depending on the clinical context.
Important Word Explanations
- Parathyroid Glands: Small glands behind the thyroid that regulate calcium balance
- Hyperparathyroidism: Excess parathyroid hormone production
- Hypoparathyroidism: Reduced parathyroid hormone production
- Hypocalcemia: Low blood calcium levels
- Hypercalcemia: High blood calcium levels
- Calcitriol: Active form of vitamin D produced in the kidneys
- Malabsorption: Reduced nutrient absorption from the intestines
~END~
Related Posts
None found

Cool blog.