Overview
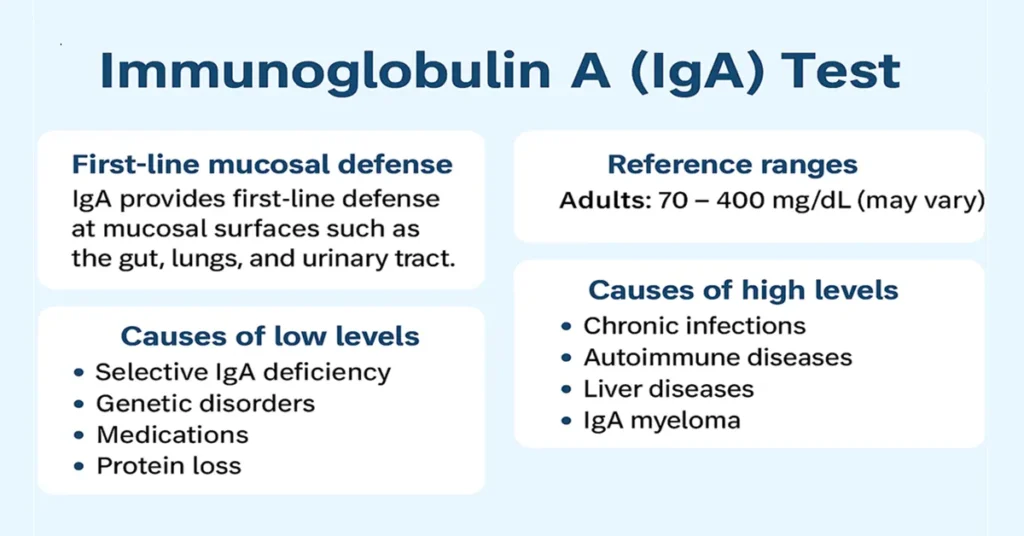
Immunoglobulin A (IgA) is one of the five major antibodies produced by the immune system (IgG, IgA, IgM, IgD, and IgE). Its primary role is to protect body surfaces that are regularly exposed to the external environment. These include the nose, mouth, lungs, digestive tract, urinary tract, and reproductive tract.
Unlike antibodies that mainly circulate in the bloodstream, IgA is especially concentrated in mucous membranes and body secretions such as saliva, tears, mucus, breast milk, and fluids lining the respiratory and intestinal tract. Because of this location, IgA acts as a frontline defender, helping prevent germs from entering the body at these vulnerable entry points.
The IgA blood test measures the level of Immunoglobulin A in the bloodstream. Clinically, it is used when doctors evaluate immune function, recurrent infections, digestive disorders, and certain autoimmune conditions, including celiac disease.
Where Is IgA Produced in the Body?
IgA is produced by plasma cells, which develop from B-lymphocytes. These plasma cells are most abundant in tissues associated with mucosal immunity, including Peyer’s patches in the small intestine, tonsils, respiratory and gastrointestinal lining, salivary glands, tear glands, and mammary glands.
IgA exists in two important forms. Serum IgA circulates in the blood and is measured in routine laboratory testing. Secretory IgA (sIgA) is found in body fluids such as saliva, tears, and breast milk and plays a major role in protecting mucosal surfaces, especially in the gut and respiratory system.
Main Functions and Importance of IgA
1. First line of defense at mucosal surfaces
IgA helps block bacteria, viruses, and toxins from attaching to and penetrating the lining of the intestines, airways, urinary tract, and reproductive organs.
2. Neutralizes pathogens
By binding to microbes, IgA prevents them from entering deeper tissues and limits their ability to cause infection.
3. Maintains healthy gut balance
IgA supports a stable intestinal environment by helping control harmful organisms while allowing beneficial bacteria to coexist.
4. Provides immunity to newborns
IgA in breast milk offers passive immune protection to infants during the early months of life, when their own immune systems are still developing.
5. Helps diagnose immune disorders
Measuring IgA supports the evaluation of immune deficiencies, chronic infections, autoimmune diseases, and conditions such as celiac disease. For this reason, the test is useful across different age groups.
Causes of Low / Negative IgA Levels
Low IgA levels can occur for several reasons and do not always indicate illness.
1. Selective IgA Deficiency
This is the most common cause and represents the most frequent primary immune deficiency worldwide. It is often inherited and may remain undetected for years.
2. Genetic immune disorders
Some inherited conditions affect the immune system’s ability to produce IgA normally.
3. Medications
Certain treatments, including immunosuppressive drugs, chemotherapy, or some anti-seizure medications, can reduce IgA levels.
4. Protein-losing conditions
Diseases that cause loss of proteins through the kidneys, intestines, or damaged tissue may also reduce IgA levels in the blood.
Symptoms of Low IgA Levels
Many individuals with low IgA levels have no noticeable symptoms, particularly those with selective IgA deficiency. When symptoms do occur, they often relate to increased vulnerability at mucosal surfaces.
Some people experience repeated sinus or chest infections, chronic digestive disturbances, or frequent gastrointestinal infections. Allergic conditions and asthma are also more common in this group. Low IgA is additionally associated with a higher likelihood of autoimmune conditions such as celiac disease, rheumatoid arthritis, or lupus.
Causes of High / Positive IgA Levels
Elevated IgA levels usually reflect long-standing immune stimulation rather than a temporary illness.
1. Chronic infections
Persistent infections, especially involving the respiratory or digestive tract, may raise IgA levels over time.
2. Autoimmune diseases
Conditions such as celiac disease, rheumatoid arthritis, and systemic lupus erythematosus are often associated with increased IgA production.
3. Liver diseases
Chronic liver conditions, including cirrhosis and long-standing hepatitis, commonly show elevated IgA levels.
4. IgA myeloma
In rare cases, very high IgA levels may be linked to IgA-producing plasma cell disorders.
Symptoms of High IgA Levels
High IgA itself does not cause symptoms. Clinical features depend on the underlying condition.
Autoimmune conditions may present with joint pain, fatigue, skin changes, or digestive complaints. Liver disease may cause jaundice, abdominal swelling, poor appetite, or general weakness. Chronic infections can lead to ongoing cough, fever, diarrhea, or persistent tiredness. In plasma cell disorders, symptoms may include bone pain, anemia, repeated infections, or unexplained weight loss.
Reference Ranges
IgA reference ranges vary with age and laboratory standards.
In adults, typical values fall between 70 and 400 mg/dL.
In children, levels are naturally lower and gradually increase with age.
Results outside the reference range are interpreted in the context of symptoms, medical history, and other immune tests.
Sample Type
IgA testing is most commonly performed on a blood sample (serum) drawn from a vein.
When evaluating mucosal immunity, secretory IgA may be assessed using saliva, stool, or breast milk samples. These tests are usually ordered for specific digestive or mucosal conditions.
Test Preparation
No special preparation is generally required for IgA testing.
Fasting is not needed.
Regular medications are usually continued unless advised otherwise.
It is helpful to inform the doctor about autoimmune conditions, chronic infections, or ongoing digestive symptoms. For children, previous medical records can assist interpretation.
When to Consult a Doctor
Medical evaluation is recommended if there are frequent sinus or chest infections, persistent digestive problems, symptoms suggestive of celiac disease, chronic fatigue with joint pain, or signs of liver disease. Children with delayed growth or repeated infections also benefit from immune assessment.
Doctors often order IgA together with IgG and IgM to gain a complete picture of immune function.
Important Word Explanations
- Antibody – A protein made by the immune system to recognize and respond to germs.
- Mucosal surfaces – Body linings such as the gut, lungs, nose, and urinary tract.
- Peyer’s patches – Specialized immune tissue located in the small intestine.
- Selective IgA Deficiency – A condition in which the body produces very little or no IgA.
- Autoimmune disease – A disorder where the immune system attacks the body’s own tissues.
- sIgA – Secretory IgA found in fluids like saliva and breast milk.
~END~
Related Posts
None found