Causes of High Direct Bilirubin and How to Reduce It
What Is Direct Bilirubin?
Direct bilirubin, also called conjugated bilirubin, is the form of bilirubin that has already been processed by the liver and combined with bile. Under normal circumstances, it moves smoothly through the bile ducts into the intestine and leaves the body.
When direct bilirubin is high, it usually means that bilirubin is being produced and processed, but is not able to flow out properly. Clinically, this points doctors toward problems related to the liver’s drainage system or conditions that interfere with bile flow rather than red blood cell breakdown.
Understanding this distinction is important because it helps narrow down the cause and guides further evaluation.
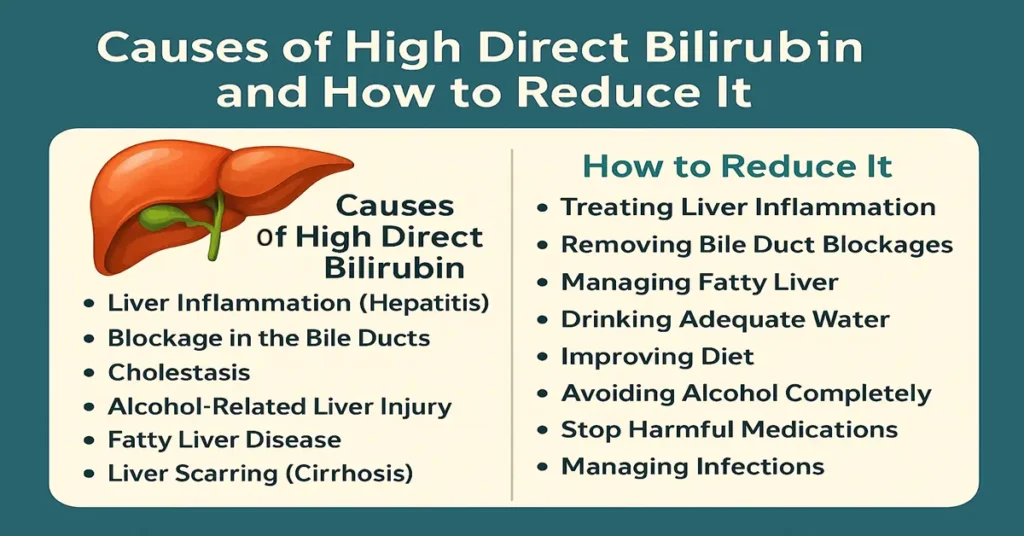
Why Does Direct Bilirubin Increase?
High direct bilirubin is most commonly linked to liver conditions or obstruction to bile flow. In day-to-day lab practice, these are the situations where conjugated bilirubin tends to rise.
Liver inflammation (hepatitis)
When the liver is inflamed due to viral infection, alcohol, drug toxicity, or autoimmune causes, it loses efficiency in moving bilirubin into bile. As a result, conjugated bilirubin leaks back into the bloodstream.
Blockage in the bile ducts
Any obstruction along the bile ducts prevents bilirubin from reaching the intestine. Gallstones are a common cause, but narrowing of ducts, enlarged lymph nodes, pancreatic or bile duct tumors, and thickened bile in very ill or dehydrated patients are also seen. Clinically, this often presents with pale stools and dark urine.
Cholestasis (reduced bile flow)
Cholestasis means bile flow is slowed or stopped. It can occur within the liver (intrahepatic) or outside it (extrahepatic). Pregnancy, certain medications, and liver diseases are common triggers. In routine practice, itching is often an early symptom.
Alcohol-related liver injury
Regular or heavy alcohol intake inflames liver cells and interferes with bile movement. Even before advanced damage develops, direct bilirubin may start rising.
Fatty liver disease
Both non-alcoholic and alcohol-related fatty liver can disturb bile formation and transport. In many patients, this is detected incidentally during routine blood tests.
Liver scarring (cirrhosis)
In advanced liver disease, the normal structure of the liver becomes distorted. This mechanical disruption blocks bile channels, causing conjugated bilirubin to accumulate in the blood.
Genetic transport disorders
Rare inherited conditions such as Dubin–Johnson syndrome and Rotor syndrome affect how conjugated bilirubin is transported. These usually cause mild but persistent elevation and are often discovered incidentally.
Certain medications
Some drugs interfere with bile secretion or liver transport mechanisms. These include anabolic steroids, certain antibiotics, oral contraceptives in susceptible individuals, antifungal medicines, and chemotherapy agents.
Severe infections
Serious infections like sepsis, typhoid, or leptospirosis can temporarily impair liver function. In such cases, direct bilirubin often rises along with other liver markers and improves as the infection settles.
Symptoms of High Direct Bilirubin
Symptoms depend on how high the level is and how quickly it rises. Many patients notice:
Yellowing of the eyes and skin
Dark yellow or brown urine
Fatigue or weakness
Loss of appetite or nausea
Right-sided abdominal discomfort or heaviness
Pale or clay-colored stools
Itchy skin
Clinically, pale stools and itching are strong clues pointing toward bile flow problems rather than blood-related causes.
How to Reduce High Direct Bilirubin
Direct bilirubin levels fall only when the underlying cause is addressed. The approach depends on what is interfering with bile flow or liver function.
Managing liver inflammation
When hepatitis or liver injury is responsible, improvement usually follows appropriate medical management and removal of the triggering factor, such as alcohol or a harmful medication.
Relieving bile duct obstruction
If gallstones, strictures, or tumors are blocking bile ducts, imaging and procedures may be required to restore bile flow. Once drainage improves, direct bilirubin often falls.
Addressing fatty liver
Improvement in fatty liver reduces ongoing liver stress and helps normalize bile movement over time.
Maintaining adequate hydration
Dehydration can thicken bile and slow its flow. In routine practice, ensuring proper fluid intake often supports recovery in mild cases.
Dietary support for the liver
Light, balanced meals reduce metabolic load on the liver. Very heavy, oily foods may worsen symptoms in people with cholestasis.
Avoiding alcohol
When bilirubin is elevated, alcohol further slows bile processing and delays recovery.
Medication review
If a drug is contributing to liver stress, doctors may adjust or change it. Medications should never be stopped without medical advice.
Treating infections
When infection is the cause, direct bilirubin usually improves once the infection is properly managed.
When High Direct Bilirubin Becomes Dangerous
Doctors become concerned when direct bilirubin continues to rise or is accompanied by warning signs such as:
Rapidly worsening jaundice
Very dark urine and completely pale stools
Persistent or severe abdominal pain
Fever with jaundice
Unexplained weight loss
Confusion or excessive sleepiness
These features suggest significant liver dysfunction or complete bile obstruction and require urgent medical attention.
Test Preparation
Direct bilirubin testing usually does not require fasting. Inform the doctor or lab about all medications being taken. Alcohol should be avoided for at least 24–48 hours before testing. Staying well hydrated helps ensure reliable results. If imaging or procedures like ultrasound or ERCP are planned, those tests may have separate preparation instructions.
When to Consult a Doctor
Medical evaluation is important if yellowing of the eyes or skin appears, direct bilirubin remains above normal on repeat tests, urine darkens, stools lose color, or symptoms such as abdominal pain, fatigue, or nausea persist. People with known liver or gallbladder disease should seek early care if values change.
Important Word Explanations
Conjugated (direct) bilirubin: Bilirubin processed by the liver and mixed with bile
Cholestasis: Reduced or blocked bile flow
Hepatitis: Inflammation of the liver
Cirrhosis: Permanent scarring of the liver
ERCP: A procedure used to diagnose and treat bile duct blockages
People Also Ask
Is high direct bilirubin always serious?
Not always. Mild elevations can be temporary, but persistent or rising levels need evaluation.
Can direct bilirubin increase temporarily?
Yes. Dehydration, infections, or certain medications can cause short-term increases.
Does high direct bilirubin always mean liver disease?
No. It can also result from bile duct blockage even when liver cells are working.
When do doctors worry most about direct bilirubin?
Concern rises when levels increase rapidly or are linked with pale stools, dark urine, or pain.
Is repeat testing common for direct bilirubin?
Yes. Repeat tests help track trends and response to management.
Can direct bilirubin return to normal on its own?
It can, if the underlying cause is temporary and resolves on its own.
~END~

Such a clear and patient-friendly guide. I wish every medical website explained blood tests like this!