Overview
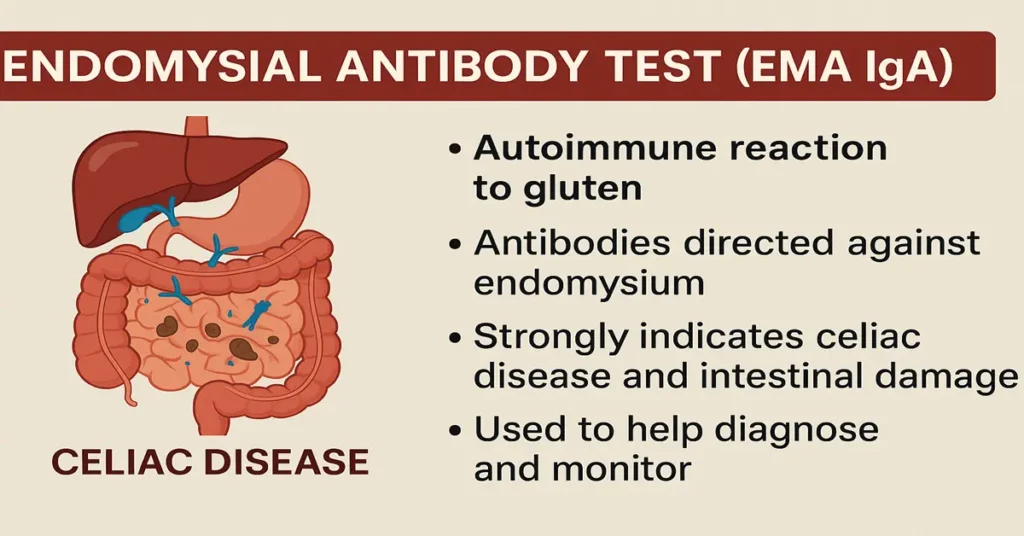
The Endomysial Antibody Test (EMA IgA) is a highly specific blood test mainly used to diagnose celiac disease, an autoimmune condition in which the body reacts abnormally to gluten. Gluten is a protein found in wheat, barley, and rye.
In people with celiac disease, eating gluten triggers the immune system to produce certain antibodies. One of the most important of these is EMA IgA, which targets the endomysium, a connective tissue layer surrounding muscle fibers.
In routine clinical practice, a positive EMA IgA result is considered very strong evidence of celiac disease, especially when the patient is consuming gluten at the time of testing. Because this test has extremely high specificity, doctors often use it to confirm celiac disease when screening tests such as tTG IgA are positive or when results are unclear.
This guide explains the EMA IgA test in clear, practical terms so that patients, students, and healthcare readers can understand what the result really means and how doctors interpret it.
What Is the Endomysial Antibody Test (EMA IgA)?
The EMA IgA test checks for endomysial IgA antibodies in the blood. These antibodies are produced when the immune system reacts against gluten and mistakenly attacks the body’s own tissues, particularly the lining of the small intestine.
From a laboratory perspective, this test is known for being:
Highly specific, with very few false positives
Most useful for confirming celiac disease
Helpful in assessing dietary compliance in diagnosed patients
EMA IgA is usually ordered after an initial screening test, most commonly tTG IgA, especially if those results are borderline or do not fully match the patient’s symptoms.
Where Is EMA IgA Produced in the Body?
EMA IgA antibodies are produced by the immune system, mainly by plasma cells, when gluten exposure triggers an autoimmune response.
Clinically, the process looks like this:
Gluten enters the small intestine
In susceptible individuals, gluten triggers inflammation
The immune system produces autoantibodies, including EMA IgA
These antibodies target the endomysium and are closely linked to intestinal damage
Under normal conditions, these antibodies are not present. Their appearance indicates autoimmune activity related to gluten exposure.
Why Is the EMA IgA Test Important?
The EMA IgA test plays a key role in both diagnosis and follow-up of celiac disease.
Detects Autoimmune Activity Related to Celiac Disease
EMA IgA antibodies are strongly linked to immune-mediated injury of the small intestine.
Confirms Gluten-Sensitive Enteropathy
A positive result usually reflects damage to intestinal villi, which are essential for nutrient absorption.
Used Along with Other Celiac Tests
Doctors often interpret EMA IgA together with:
tTG IgA
Total IgA levels
tTG IgG or DGP IgG (in IgA deficiency)
Using these tests together improves diagnostic confidence.
Helps Guide Clinical Decisions
A confirmed positive EMA IgA result often leads doctors to proceed with further evaluation, such as intestinal biopsy, or to reinforce strict dietary management.
Useful for Monitoring Gluten Exposure
In diagnosed patients:
EMA levels fall when gluten is strictly avoided
Rising or persistent positivity suggests ongoing gluten exposure
In practice, this makes EMA IgA a reliable marker of dietary adherence.
Causes of Low or Negative EMA IgA Levels
A negative EMA IgA result can occur for several reasons.
No Celiac Disease
This is the most common and expected finding in healthy individuals.
Very Early Celiac Disease
In early stages, antibody levels may be too low to detect.
Gluten-Free Diet Before Testing
If gluten has already been removed from the diet, antibody levels may decline, leading to a negative result.
IgA Deficiency
Some individuals have low or absent IgA production. In such cases:
EMA IgA may be falsely negative
Alternative tests like tTG IgG or DGP IgG are required
This is why total IgA is often checked alongside EMA testing.
Symptoms Despite a Negative Result
A negative EMA result does not cause symptoms by itself.
However, if symptoms suggest celiac disease despite a negative test, doctors may recommend further evaluation or alternative testing.
Common symptoms that prompt further investigation include bloating, altered bowel habits, unexplained anemia, weight loss, and fatigue.
Causes of High or Positive EMA IgA Levels
A positive EMA IgA result almost always reflects active celiac disease.
Autoimmune Reaction to Gluten
The immune system produces antibodies directed against the endomysium when gluten is consumed.
Continued Gluten Intake in Diagnosed Patients
In patients already diagnosed with celiac disease, persistent or rising EMA levels usually indicate ongoing gluten exposure.
Rare Exceptions
Very rarely, weak positivity may be seen in other autoimmune conditions, but this is uncommon. In routine lab practice, EMA IgA positivity is considered highly specific for celiac disease.
Symptoms Associated with Positive EMA IgA
Symptoms reflect intestinal damage rather than the antibody itself.
Digestive symptoms may include chronic diarrhea, constipation, bloating, abdominal pain, and pale bulky stools due to fat malabsorption.
Nutritional deficiency symptoms may include weight loss, fatigue, iron-deficiency anemia, and vitamin deficiencies.
Skin and bone symptoms may include dermatitis herpetiformis, bone pain, or early osteoporosis.
In children, poor growth, delayed development, or short stature may be seen.
Reference Ranges
EMA IgA results are usually reported qualitatively.
Negative
No endomysial antibodies detected
Positive
Endomysial antibodies detected, strongly suggestive of celiac disease
Some laboratories also report titers such as 1:10 or 1:40. Higher titers generally reflect stronger autoimmune activity.
Sample Type
The test requires a blood sample.
Serum IgA autoantibodies are measured.
No stool or urine sample is involved.
How the Test Is Performed
A blood sample is collected
Indirect immunofluorescence is used to detect antibodies
Results are reported as positive or negative, sometimes with titers
This method is technically demanding but offers very high specificity.
Test Preparation
Continue eating gluten before testing, as stopping gluten can cause false-negative results.
No fasting is required.
Inform your doctor if IgA deficiency is suspected.
Also tell your doctor about immunosuppressive medicines, steroids, or known autoimmune conditions, as these may influence results.
When to Consult a Doctor
Medical advice is recommended if:
You develop symptoms after eating gluten-containing foods
You have unexplained anemia, fatigue, or weight loss
A close family member has celiac disease
Your EMA IgA test is positive
Symptoms persist despite a gluten-free diet
You are known to have IgA deficiency
Urgent evaluation is needed in cases of severe abdominal pain, persistent vomiting, uncontrolled diarrhea, or poor growth in children.
Important Word Explanations
Endomysium: Connective tissue surrounding muscle fibers
Autoantibodies: Antibodies directed against the body’s own tissues
Gluten: Protein found in wheat, barley, and rye
Celiac disease: Autoimmune reaction to gluten
IgA deficiency: Low or absent Immunoglobulin A
Enteropathy: Disease of the intestines
Titer: A measure of antibody strength in the blood
People Also Ask
Is a positive EMA IgA result serious?
It strongly suggests celiac disease and should be evaluated further by a doctor.
Can EMA IgA be temporarily negative?
Yes. Early disease or avoiding gluten before testing can cause a negative result.
Does a positive EMA IgA always mean celiac disease?
In most cases, yes. The test is highly specific for celiac disease.
When do doctors usually order EMA IgA?
When screening tests are positive or unclear, or to confirm suspected celiac disease.
Is repeat testing of EMA IgA common?
Yes, especially to monitor dietary compliance in diagnosed patients.
Can EMA IgA become negative again?
Yes. With strict gluten avoidance, antibody levels usually fall over time.
~END~
Related Posts
None found