What is the Direct Coombs Test (DAT)?
The Direct Coombs Test, also called the Direct Antiglobulin Test (DAT), is a laboratory blood test used to check whether antibodies or complement proteins are already attached to the surface of red blood cells.
In day-to-day clinical practice, this test helps doctors understand why red blood cells may be breaking down earlier than normal. It is especially useful when anemia is present and routine causes do not fully explain the findings. Rather than measuring red blood cell levels directly, the test looks for immune activity happening on the red blood cells themselves.
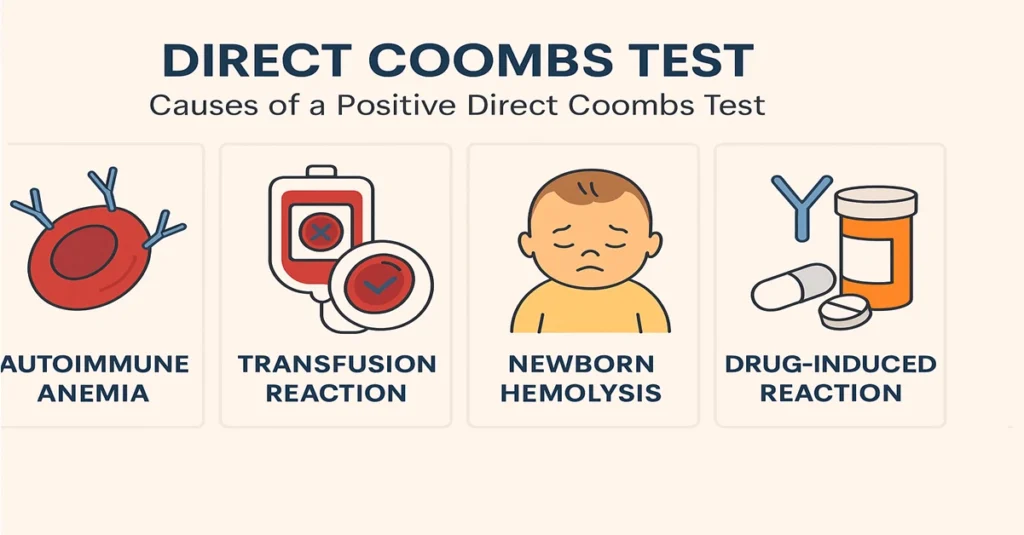
A positive result suggests that the immune system is reacting against red blood cells, which can be seen in certain autoimmune conditions, transfusion-related reactions, or specific situations in newborns. A negative result reassures doctors that immune-mediated red cell destruction is unlikely.
Where It Is Synthesized or Produced in the Body
The Direct Coombs Test is not something produced by the body. It is a laboratory procedure performed on a blood sample.
In the laboratory, a prepared reagent known as antihuman globulin (Coombs reagent) is used. This reagent is designed to react with antibodies or complement proteins if they are already attached to red blood cells in the patient’s sample. When such immune components are present, the reagent causes the red blood cells to clump together, a visible reaction that confirms a positive test.
From a laboratory perspective, this reaction is straightforward, but clinically it provides important insight into immune activity that cannot be seen on a routine blood count.
Main Functions and Importance of the Direct Coombs Test
The Direct Coombs Test has a specific and focused role in medical diagnostics. It is mainly used to identify immune-mediated red blood cell destruction and to guide further evaluation when anemia or jaundice is unexplained.
Clinically, it helps doctors confirm whether anemia is related to an immune process rather than nutritional deficiency, blood loss, or bone marrow problems. It is also an important investigation tool after blood transfusions, where unexpected immune reactions need to be identified early. In newborn care, it supports the evaluation of jaundice or anemia related to blood group incompatibility.
Overall, the test is commonly used in hematology, transfusion medicine, and neonatal settings, where understanding immune involvement is critical for accurate diagnosis.
Causes of Low or Negative Levels
A negative Direct Coombs Test means that no antibodies or complement proteins are detected on the red blood cells. From a clinical point of view, this is considered a normal and reassuring result.
This finding is typically seen in healthy individuals and in patients whose anemia is due to non-immune causes. It may also be observed in people who previously had immune-related hemolysis but are no longer showing active immune attachment on red blood cells at the time of testing.
Symptoms of Low or Negative Levels
There are no symptoms specifically linked to a negative Direct Coombs Test. The result simply indicates that the immune system is not attacking red blood cells.
If a person has anemia with a negative result, doctors usually look toward other explanations, such as nutritional deficiencies, chronic illness, or bone marrow-related conditions, rather than immune destruction.
Causes of High or Positive Levels
A positive Direct Coombs Test indicates that antibodies or complement proteins are present on red blood cells, pointing toward immune-mediated hemolysis.
In clinical practice, this result may be seen in autoimmune hemolytic anemia, following incompatible blood transfusions, or in newborns affected by blood group incompatibility. Certain medications and underlying immune or blood-related disorders can also be associated with a positive result. Doctors interpret this finding alongside the patient’s history, symptoms, and other laboratory results to understand the underlying reason.
Symptoms of High or Positive Levels
The Direct Coombs Test itself does not cause symptoms. Any symptoms arise from the breakdown of red blood cells rather than from the test result.
Patients with immune-related hemolysis may show signs of anemia, such as tiredness, weakness, or shortness of breath. Jaundice may appear due to increased bilirubin released from destroyed red blood cells, and urine may become darker in some cases. In longer-standing conditions, enlargement of the spleen may also be noted during clinical examination.
Doctors often consider a Direct Coombs Test when these features appear without an obvious explanation.
Reference Ranges for Direct Coombs Test
The Direct Coombs Test is reported as either negative or positive, rather than as a numerical value.
A negative result indicates no detectable immune attachment on red blood cells.
A positive result confirms the presence of antibodies or complement, supporting an immune-mediated process.
This clear binary reporting makes the test easy to interpret when correlated with clinical findings.
Sample Type and Test Procedure
The test is performed on a sample of whole blood collected from a vein, usually into an EDTA anticoagulant tube.
In the laboratory, red blood cells are separated and washed to remove free antibodies. The Coombs reagent is then added. If immune components are already attached to the red blood cells, visible clumping occurs, confirming a positive reaction. The procedure is routine in hospital and diagnostic laboratories and does not take long to complete.
Test Preparation
No special preparation is needed for this test. Fasting is not required.
However, it is important to inform the doctor about recent blood transfusions, ongoing medications, or recent infections, as these factors can influence how results are interpreted. In newborns, the test is usually performed soon after birth when anemia or jaundice is clinically noted.
When to Consult a Doctor
A doctor should be consulted if there are unexplained signs of anemia, such as persistent fatigue, jaundice, or dark-colored urine. Medical review is also important after blood transfusions if new symptoms develop, or in newborns who show early jaundice or low hemoglobin levels.
The Direct Coombs Test helps doctors clarify whether the immune system is involved and supports timely, appropriate clinical decisions.
Important Word Explanations
- Antibody: A protein produced by the immune system that targets specific substances.
- Complement: A group of immune proteins that work with antibodies to damage or remove cells.
- Hemolysis: The breakdown of red blood cells before their normal lifespan ends.
- Autoimmune Hemolytic Anemia (AIHA): A condition where the immune system attacks its own red blood cells.
- Rh Incompatibility: A blood group mismatch between mother and baby that can lead to newborn anemia or jaundice.
~END~
Related Posts
None found