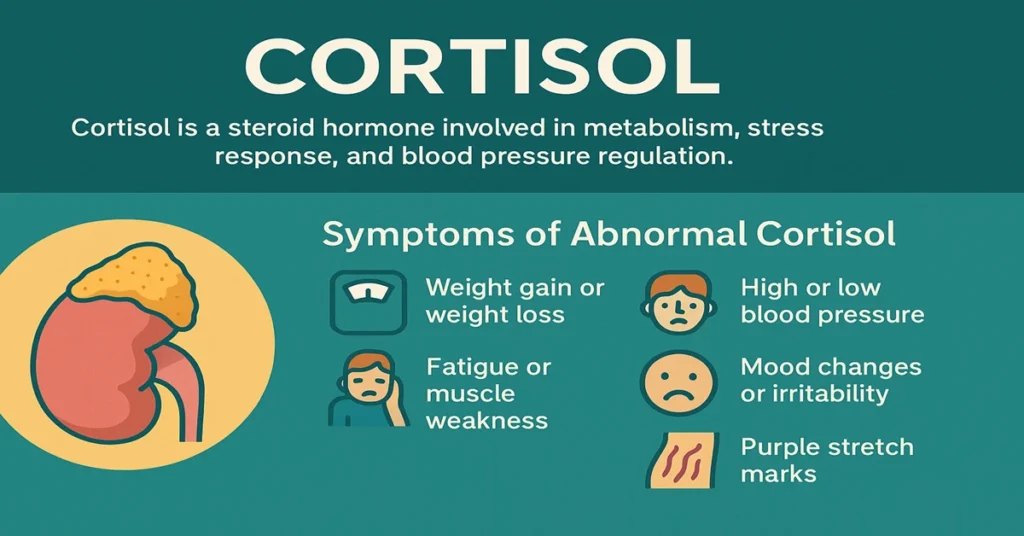
The Cortisol Test measures the level of cortisol, a steroid hormone often referred to as the body’s primary stress hormone. Cortisol levels naturally rise during physical or emotional stress, but the hormone also plays a steady, day-to-day role in keeping many vital systems working normally.
In clinical practice, this test is commonly used to assess adrenal gland function and to investigate hormonal imbalances linked to conditions such as Cushing’s syndrome or Addison’s disease. It also helps doctors understand how the body is responding to prolonged stress or illness.
What Is Cortisol?
Cortisol is a glucocorticoid hormone, belonging to the steroid hormone family. It is essential for maintaining balance within the body, particularly in how energy is produced and used.
When the body faces stress—whether from infection, injury, emotional strain, or surgery—the brain signals the adrenal glands to release cortisol. This response helps maintain blood sugar levels, supports blood pressure, and keeps inflammation under control. In normal circumstances, cortisol follows a predictable daily rhythm and quietly supports routine body functions.
Problems arise when cortisol levels stay too high or fall too low for prolonged periods. For this reason, measuring cortisol is a valuable tool in hormonal and adrenal evaluations.
Where It Is Produced in the Body
Cortisol is produced in the adrenal cortex, specifically in the zona fasciculata, the middle layer of the adrenal glands. These glands sit just above each kidney and are part of the endocrine system.
Its production is regulated by a tightly controlled feedback system involving:
- The hypothalamus, which releases corticotropin-releasing hormone (CRH)
- The pituitary gland, which releases adrenocorticotropic hormone (ACTH)
- The adrenal glands, which release cortisol in response to ACTH
This system—known as the hypothalamic–pituitary–adrenal (HPA) axis—ensures cortisol levels rise and fall appropriately throughout the day.
Main Functions and Importance
Cortisol influences many organs and tissues, often in subtle but important ways. It supports metabolism by helping the body convert fats, proteins, and carbohydrates into usable energy. It also plays a role in maintaining blood pressure and supporting cardiovascular stability.
Another key function is immune regulation. Cortisol helps limit excessive inflammation, preventing the immune system from causing unnecessary tissue damage. It also contributes to the normal sleep–wake rhythm, with levels highest in the early morning and lowest late at night.
From a clinical standpoint, cortisol reflects how well the body adapts to stress and maintains internal balance.
Causes of Low Cortisol Levels
Low cortisol levels usually suggest reduced adrenal hormone production or impaired stimulation from the pituitary gland. This pattern is often seen in adrenal insufficiency or disorders affecting hormonal control pathways.
Common clinical associations include Addison’s disease, pituitary dysfunction, or suppression of adrenal activity following long-term corticosteroid use. Infections or autoimmune damage to the adrenal glands may also reduce cortisol output.
Doctors typically interpret low cortisol results alongside symptoms and other hormone tests rather than in isolation.
Symptoms of Low Cortisol Levels
When cortisol is consistently low, the body may struggle to maintain energy levels, blood pressure, and metabolic balance. Patients often report persistent fatigue, weakness, dizziness—especially on standing—and unintended weight loss.
In some cases, gastrointestinal discomfort, low appetite, or changes in skin pigmentation may be noted. These features guide further evaluation rather than serving as a diagnosis on their own.
Causes of High Cortisol Levels
Elevated cortisol levels usually reflect prolonged stimulation of the adrenal glands. This may occur in conditions such as Cushing’s syndrome or Cushing’s disease, where cortisol production is increased due to adrenal or pituitary causes.
Chronic physical or psychological stress can also lead to sustained elevations. In addition, long-term use of corticosteroid medications may raise measured cortisol levels or interfere with normal regulation.
Symptoms of High Cortisol Levels
Persistently high cortisol affects multiple body systems. Clinically, this may be reflected by changes in body fat distribution, elevated blood pressure, impaired glucose control, and skin changes.
Patients may also experience muscle weakness, mood changes, or reduced resistance to infections. These findings prompt further testing to identify the underlying cause of cortisol excess.
Reference Ranges
Cortisol follows a strong daily rhythm, so reference ranges depend on the time of sample collection. Typical values (which may vary slightly between laboratories) are:
- Morning (around 8 a.m.): 5–25 µg/dL (138–690 nmol/L)
- Afternoon (around 4 p.m.): 2–14 µg/dL (55–386 nmol/L)
Results are always interpreted in relation to timing, clinical symptoms, and other hormone levels.
Sample Types and Testing Methods
Cortisol can be measured using different sample types, depending on the clinical question.
Blood (serum) testing is the most common and is often done in the morning or evening to assess daily variation.
A 24-hour urine collection measures total cortisol excretion over a full day and is useful in evaluating sustained overproduction.
Saliva testing, usually collected late at night, reflects free cortisol levels and helps assess abnormal nighttime secretion.
Test Preparation
Because cortisol levels fluctuate during the day, timing is important. Patients should follow the collection time recommended by their doctor.
It is important to inform the healthcare provider about all medications being taken, particularly steroids or hormone therapies, as these can affect results. Avoiding intense physical activity and significant stress before testing can help reduce temporary fluctuations.
When to Consult a Doctor
Medical advice should be sought if there is ongoing fatigue, unexplained weight changes, abnormal blood pressure, or symptoms suggesting adrenal or hormonal imbalance.
If cortisol levels fall outside the expected range, doctors may recommend additional hormone tests or dynamic studies to clarify adrenal and pituitary function and to guide further evaluation.
Important Word Explanations
- Cortisol: A steroid hormone involved in stress response and metabolism
- Glucocorticoid: A class of hormones that regulate glucose metabolism and inflammation
- Adrenal Glands: Hormone-producing glands located above the kidneys
- ACTH: A pituitary hormone that stimulates cortisol release
- Cushing’s Syndrome: A condition associated with excess cortisol
- Addison’s Disease: A condition caused by insufficient cortisol production
- HPA Axis: The hormonal control system linking the brain and adrenal glands
~END~
Related Posts
None found