Chloride (Cl⁻) Test: Meaning, Functions, Causes, Symptoms, Normal Range & Complete Guide
Overview
Chloride (Cl⁻) is a key electrolyte in the human body and carries a negative electrical charge. It works closely with sodium (Na⁺) and potassium (K⁺) to maintain fluid balance, support normal nerve and muscle activity, and keep the body’s internal environment stable. Although chloride often receives less attention than sodium or potassium, it plays an equally important role in maintaining normal physiology.
A Chloride Blood Test measures the amount of chloride circulating in the bloodstream. It is routinely included in an Electrolyte Panel or Basic Metabolic Panel (BMP). Clinically, chloride levels help doctors assess hydration status, kidney performance, and acid–base balance. Because chloride changes often parallel sodium and bicarbonate shifts, this test is especially useful when evaluating metabolic disturbances, kidney conditions, lung disorders, and fluid imbalances.
What is Chloride (Cl⁻)?
Chloride is a negatively charged ion found mainly in the fluid outside body cells. Its primary role is to help regulate the movement of water between different body compartments. Chloride also works alongside sodium to maintain blood volume and pressure, and with bicarbonate to keep blood acidity within a healthy range.
In addition, chloride is essential for the production of hydrochloric acid in the stomach, which supports digestion and nutrient absorption. Because of its close relationship with sodium and water balance, changes in chloride levels often reflect shifts in hydration or kidney regulation rather than isolated chloride disorders.
Where is Chloride Obtained and Regulated in the Body?
The body does not produce chloride on its own. It is obtained entirely from dietary sources, with common salt (sodium chloride) being the main contributor. Many everyday foods naturally contain chloride or have it added during processing.
After absorption from the intestines, chloride circulates in the blood and extracellular fluid. The kidneys then carefully regulate chloride by adjusting how much is reabsorbed or excreted in urine. Hormones, particularly aldosterone, influence this process. When fluid loss, kidney dysfunction, or hormonal imbalance occurs, chloride levels may shift accordingly.
Main Functions and Importance of Chloride
Helps Maintain Fluid Balance
Chloride plays a central role in regulating water distribution inside and outside cells. Together with sodium and potassium, it helps maintain proper hydration and prevents abnormal fluid accumulation or depletion.
Regulates Acid–Base Balance (pH)
Chloride works in balance with bicarbonate to keep blood pH stable. When chloride levels fall, bicarbonate may rise, leading to a more alkaline state. When chloride rises, bicarbonate may decrease, contributing to acidosis. This balance is critical for normal enzyme and metabolic activity.
Supports Nerve and Muscle Function
Chloride contributes to the electrical environment required for nerve signaling and muscle contraction. Proper levels help ensure coordinated muscle movement and stable heart rhythm.
Aids in Digestion
Chloride is a key component of hydrochloric acid in the stomach. Adequate chloride levels support effective digestion, protect against ingested bacteria, and assist in the absorption of nutrients such as iron and vitamin B12.
Causes of Low Chloride (Hypochloremia)
Hypochloremia refers to chloride levels below the normal range. It most often develops due to fluid loss, dilution, or disturbances in acid–base balance rather than a primary chloride deficiency.
Low chloride is commonly seen in situations involving prolonged vomiting, excessive fluid intake, certain heart or lung conditions, and the use of medications that increase urinary losses. In many cases, low chloride reflects an underlying metabolic or hydration-related issue.
Symptoms of Low Chloride (Hypochloremia)
Symptoms depend on how quickly and how far chloride levels fall. Mild reductions may cause few noticeable effects, while more significant drops can affect muscles and mental clarity.
People may experience fatigue, muscle weakness or cramps, dizziness, or difficulty concentrating. When hypochloremia is associated with acid–base disturbances, breathing changes or heart rhythm abnormalities may also occur.
Causes of High Chloride (Hyperchloremia)
Hyperchloremia occurs when chloride levels rise above the normal range. This usually reflects water loss, reduced kidney excretion, or metabolic acidosis rather than excessive chloride intake alone.
High chloride levels are often seen in dehydration, kidney dysfunction, certain hormonal disorders, or after large volumes of saline fluids are administered. In hospitalized patients, hyperchloremia is frequently evaluated in the context of overall fluid and acid–base status.
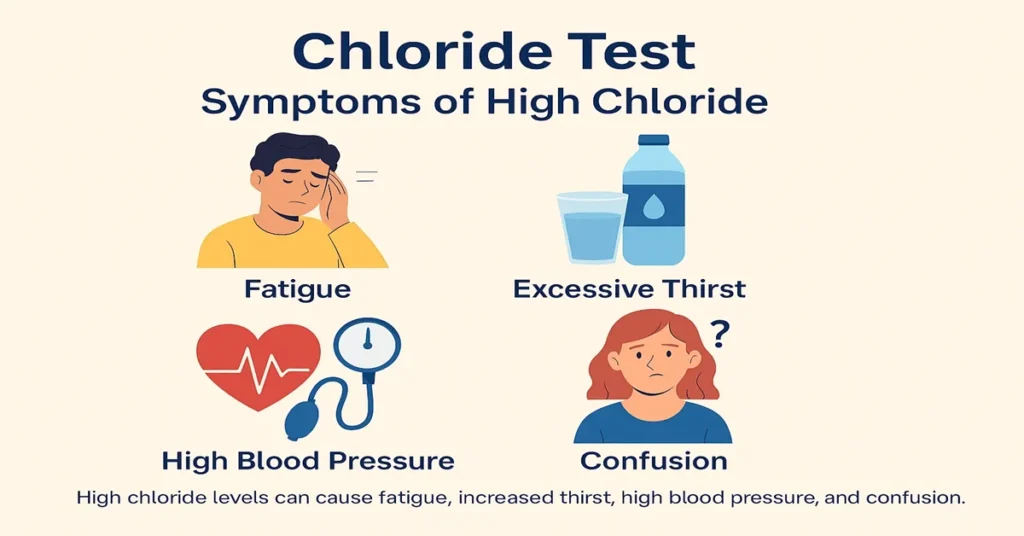
Symptoms of High Chloride (Hyperchloremia)
Symptoms are often related to the underlying condition rather than chloride itself. Individuals may notice increased thirst, dryness of the mouth, fatigue, or weakness.
In more pronounced cases, mental clouding, rapid or deep breathing, or signs of dehydration may appear. Significant hyperchloremia often signals a broader metabolic imbalance that requires medical evaluation.
Reference Range for Chloride
Typical reference values for blood chloride are:
Normal Range: 96 – 106 mmol/L
Values significantly outside this range are considered clinically important and are interpreted alongside other electrolytes and kidney markers.
Sample Type and Test Information
Sample Type: Serum
Tube Used: Red Top (Plain Tube)
Fasting: Not usually required
The test requires a simple blood draw and is commonly performed with sodium, potassium, bicarbonate, and kidney function tests.
Test Preparation
Special preparation is usually not needed unless other tests are being performed at the same time.
It is important to inform the healthcare provider about medications, recent IV fluids, or significant fluid losses, as these factors can influence chloride levels. Maintaining normal hydration before testing helps ensure accurate interpretation.
When to Consult a Doctor
Medical advice should be sought if chloride levels are abnormal or if symptoms such as persistent fatigue, confusion, muscle weakness, or breathing changes occur.
Chloride imbalances often point toward underlying conditions involving fluid balance, kidney function, or acid–base regulation. Identifying the cause is essential for appropriate management and recovery.
Important Word Explanations
Electrolyte
A mineral with an electrical charge that supports nerve signaling, muscle function, and fluid balance.
Hypochloremia
A condition in which blood chloride levels are lower than normal.
Hyperchloremia
A condition in which blood chloride levels are higher than normal.
Metabolic Acidosis
A state in which the body accumulates excess acid or cannot adequately remove it.
Hydrochloric Acid (HCl)
A strong acid in the stomach that aids digestion and nutrient absorption.
Corticosteroids
Medications that influence fluid, electrolyte, and hormonal balance.
Addison’s Disease
A disorder of the adrenal glands that affects sodium and chloride regulation.
~END~
Related Posts
None found