What is Anti-Thrombin III (AT III)?
Anti-Thrombin III (AT III), commonly called Antithrombin, is a naturally occurring protein in the blood that helps regulate clot formation. It acts as one of the body’s key internal “brakes” on the clotting system, making sure clots form only when necessary—such as after an injury—and do not develop unnecessarily inside blood vessels.
AT III works mainly by neutralizing important clotting enzymes, particularly thrombin (Factor IIa) and Factor Xa. By keeping these enzymes under control, it maintains smooth blood flow and prevents excessive clotting. When AT III levels are low or its function is reduced, the balance shifts toward clot formation, increasing the risk of conditions such as deep vein thrombosis (DVT) or pulmonary embolism (PE).
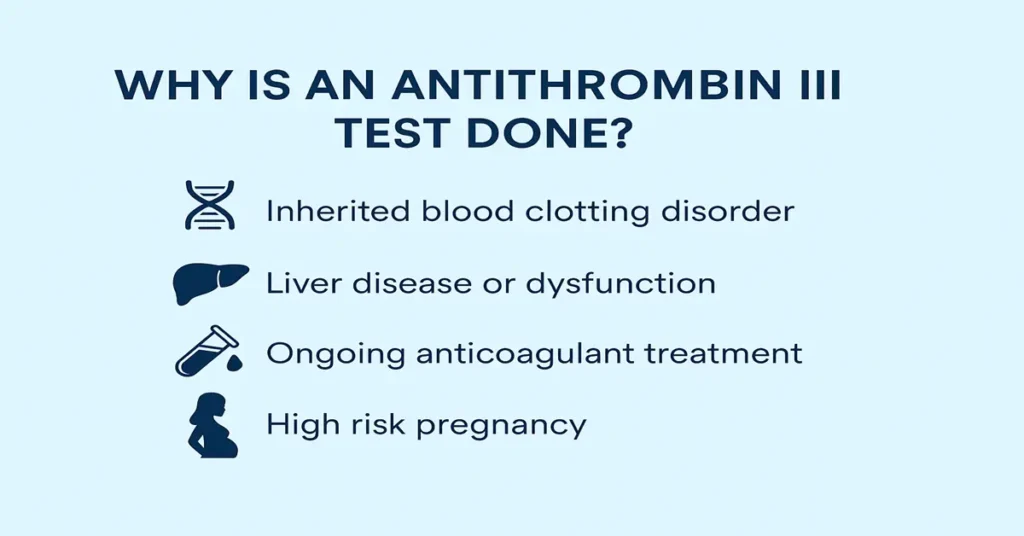
For this reason, doctors often request an AT III test in people who develop blood clots without a clear cause, at a young age, or repeatedly.
Where is Anti-Thrombin III Produced in the Body?
Anti-Thrombin III is produced primarily in the liver and then released into the bloodstream. Once in circulation, it remains active and ready to bind excess clotting enzymes whenever clotting activity becomes too strong.
Because the liver is responsible for its production, liver-related conditions can influence AT III levels. In clinical practice, this connection is always kept in mind when interpreting results.
Main Functions and Importance
Anti-Thrombin III plays a central role in maintaining normal blood clotting balance (hemostasis). It does not stop clotting altogether but keeps it appropriately controlled.
From a clinical perspective, its importance lies in three main areas. First, it limits the action of key clotting factors such as thrombin and Factor Xa, preventing unnecessary clot extension. Second, it supports the action of heparin—both the natural substance in the body and the medication—by greatly enhancing its anticoagulant effect. Third, it helps protect against harmful clots that can obstruct blood flow in veins or lungs.
When AT III activity is reduced, this protective control weakens. That is why measuring AT III becomes particularly relevant in patients with unexplained clotting events or those who respond poorly to heparin therapy.
Causes of Low Anti-Thrombin III Levels
Low AT III levels may be inherited or acquired. Inherited deficiency is uncommon and usually present from birth due to a genetic change affecting AT III production or function. People with this condition often come to medical attention because of unexpected or recurrent clotting episodes.
More commonly, low levels are acquired later in life. In these situations, AT III may be reduced because the body cannot produce enough, loses it, or consumes it during periods of intense clotting activity. Conditions affecting the liver, kidneys, or the clotting system itself are often considered when evaluating such results.
Symptoms of Low Anti-Thrombin III Levels
Low AT III levels do not cause symptoms directly. Instead, symptoms arise from the tendency toward abnormal clot formation. Clinically, this may present as leg swelling or pain, sudden breathlessness, chest discomfort, or clotting in less typical locations.
Because these events can be serious, identifying low AT III levels helps doctors understand why clotting may be occurring and guides further evaluation.
Causes of High Anti-Thrombin III Levels
Elevated AT III levels are uncommon and usually not clinically concerning. They may appear temporarily during recovery from illness, inflammation, or while a person is receiving anticoagulant therapy. In most cases, higher-than-normal levels do not indicate disease and do not require specific follow-up.
Symptoms of High Anti-Thrombin III Levels
High AT III levels themselves do not cause symptoms and are generally considered a benign laboratory finding. They are often discovered incidentally during routine testing.
Reference Ranges
AT III can be measured in two ways: by its functional activity or by its antigen (amount) level.
- Functional activity: typically around 80%–120%
- Antigen level: commonly within the laboratory’s stated reference range
Values below the lower limit suggest reduced activity or quantity. Doctors often interpret both results together to understand whether the issue is reduced production or reduced function.
Sample Type
The test is performed on a blood sample collected into a citrate tube (light blue top). This preserves clotting factors accurately for analysis.
Patients should always inform the laboratory or doctor about any anticoagulant treatment, as this context is important for correct interpretation.
Test Preparation
No fasting is required for AT III testing. However, timing in relation to anticoagulant therapy matters. Heparin and some other blood thinners can influence results, so doctors may advise specific timing for sample collection.
Providing a brief medication history helps ensure the result is interpreted correctly.
When to Consult a Doctor
AT III testing is usually considered when a person develops blood clots unexpectedly, at a young age, or repeatedly, or when there is a strong family history of clotting disorders. It is also relevant when heparin treatment does not appear to work as expected.
If results show reduced AT III levels, doctors use this information alongside clinical history and other tests to decide on further evaluation and long-term management.
Important Word Explanations
- Anticoagulant: A substance that slows or prevents blood clot formation.
- Thrombin (Factor IIa): An enzyme central to forming blood clots.
- Factor Xa: A clotting factor that activates thrombin production.
- DVT (Deep Vein Thrombosis): A clot forming in deep veins, usually in the legs.
- PE (Pulmonary Embolism): A clot that travels to and blocks blood vessels in the lungs.
- Heparin Resistance: Reduced response to heparin, often linked to low AT III levels.
~END~
Related Posts
None found