What is ACE (Angiotensin-Converting Enzyme)?
ACE, or Angiotensin-Converting Enzyme, is an enzyme that plays an important role in regulating blood pressure and fluid balance in the body. Its primary function is to convert angiotensin I, an inactive substance, into angiotensin II — an active compound that causes blood vessels to narrow and blood pressure to rise.
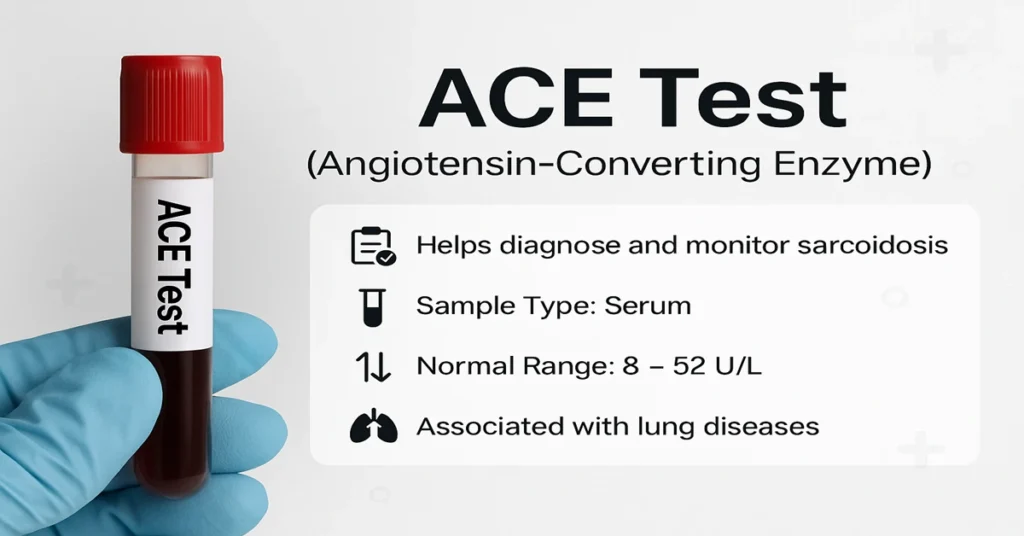
From a laboratory perspective, ACE is not measured to assess blood pressure directly. Instead, the ACE test is mainly used as a biochemical marker of certain inflammatory conditions, especially sarcoidosis. Changes in ACE levels can also be seen in some lung, liver, and thyroid disorders, which is why results are always interpreted in clinical context.
Where is ACE Produced in the Body?
ACE is produced mainly by the endothelial cells lining the blood vessels, particularly in the lungs. Smaller amounts are also produced in other tissues, including the kidneys, brain, and blood vessels throughout the body.
Because of this widespread distribution, ACE is continuously released into the bloodstream. In certain diseases — especially those involving chronic inflammation — enzyme production increases, leading to higher measurable blood levels.
Main Functions and Importance of ACE
ACE is a central component of the Renin–Angiotensin–Aldosterone System (RAAS), the body’s long-term regulatory system for blood pressure and fluid balance.
Its key role is the conversion of angiotensin I into angiotensin II, a substance that narrows blood vessels and supports blood pressure maintenance. Through this mechanism, ACE also indirectly influences aldosterone release, which affects sodium and water retention.
Clinically, however, ACE testing is most valuable as a marker of granulomatous inflammation. Elevated ACE levels are commonly associated with conditions where immune cells cluster together in tissues, such as sarcoidosis. For this reason, the test is often used to support diagnosis and to monitor disease activity over time rather than as a standalone diagnostic tool.
Causes of Low ACE Levels
Low ACE levels are less commonly encountered and are usually not concerning on their own. In clinical practice, reduced ACE activity is often linked to external factors rather than disease.
Lower levels may be seen in people taking ACE-inhibitor medications, as these drugs directly suppress enzyme activity. Certain chronic lung conditions, thyroid disorders, or inherited variations can also be associated with naturally lower ACE levels.
Symptoms of Low ACE Levels
ACE itself does not cause symptoms. When low levels are detected, any symptoms present usually relate to the underlying condition or medication effect rather than the enzyme level itself.
Patients may experience features such as dizziness, fatigue, or breathlessness depending on the broader clinical picture, but these are not specific to ACE deficiency.
Causes of High ACE Levels
Elevated ACE levels are most often associated with chronic inflammatory conditions, particularly those involving granuloma formation.
Sarcoidosis is the most common condition linked to raised ACE. Other infectious or inflammatory diseases, including certain lung infections and occupational lung disorders, can also increase ACE production. In these conditions, immune cells within granulomas release larger amounts of the enzyme into circulation.
Because ACE elevation is not disease-specific, results must always be interpreted alongside imaging findings, clinical symptoms, and other laboratory tests.
Symptoms of High ACE Levels
ACE elevation itself does not cause symptoms. Any symptoms experienced are due to the underlying inflammatory or infectious condition.
Depending on organ involvement, patients may report respiratory symptoms, skin changes, fatigue, weight loss, or systemic features such as fever. The pattern and severity vary widely and guide further evaluation.
Reference Range
ACE reference ranges differ slightly between laboratories and testing methods. A commonly used adult reference range is:
- 8 – 52 U/L
Values above this range may raise suspicion for sarcoidosis or other granulomatous conditions, but they are not diagnostic on their own. Serial measurements are often more useful than a single result.
Sample Type and Handling
The ACE test is performed on serum obtained from a blood sample.
Blood is collected in a plain red-top tube or a serum separator tube. No special handling beyond standard serum processing is usually required. The enzyme remains stable under routine laboratory conditions.
How the ACE Test is Performed
A blood sample is drawn from a vein, usually from the arm. After clotting, the sample is centrifuged to separate serum.
The laboratory then measures ACE activity using biochemical methods. Results are compared with the laboratory’s reference range and interpreted in combination with clinical findings.
Interpreting ACE Test Results
Normal ACE levels generally suggest the absence of active granulomatous inflammation, although they do not rule out disease.
Elevated levels support the possibility of sarcoidosis or similar inflammatory conditions, particularly when clinical and imaging findings align. Low levels are most often related to medication use or non-inflammatory conditions.
Clinicians focus on trends over time, especially when monitoring known sarcoidosis, rather than relying on a single value.
Test Preparation
No fasting is required for the ACE test.
Patients should inform their doctor about current medications, especially ACE inhibitors, as these can significantly lower enzyme levels. Routine daily activities usually do not interfere with testing.
When to Consult a Doctor
Medical review is advised if symptoms such as persistent cough, unexplained breathlessness, skin lesions, fatigue, weight loss, fever, or night sweats are present.
ACE testing is most helpful when used alongside imaging studies and other investigations to clarify the cause of chronic inflammation.
Important Word Explanations
- Enzyme: A protein that speeds up chemical reactions in the body
- Vasoconstriction: Narrowing of blood vessels, which increases blood pressure
- Aldosterone: A hormone that regulates sodium and water balance
- Granuloma: A small cluster of immune cells formed during long-standing inflammation
- Sarcoidosis: An inflammatory disease that causes granulomas, commonly in the lungs
- RAAS: The hormone system that helps regulate blood pressure and fluid balance
~END~